76-Year-Old Woman With a Bluish-Purple Lump in her Left Upper Medial Leg
Test your diagnostic knowledge with this month's Image IQ.
Copur is a medical oncologist/ hematologist at Morrison Cancer Center, Mary Lanning Healthcare in Hastings, Nebraska, and is a professor at the University of Nebraska Medical Center in Omaha, Nebraska. He is also editor-at-Large and a Community Oncology Advisory Board member at ONCOLOGY.

Wedel is a staff pathologist at Mary Lanning Healthcare.

Presentation
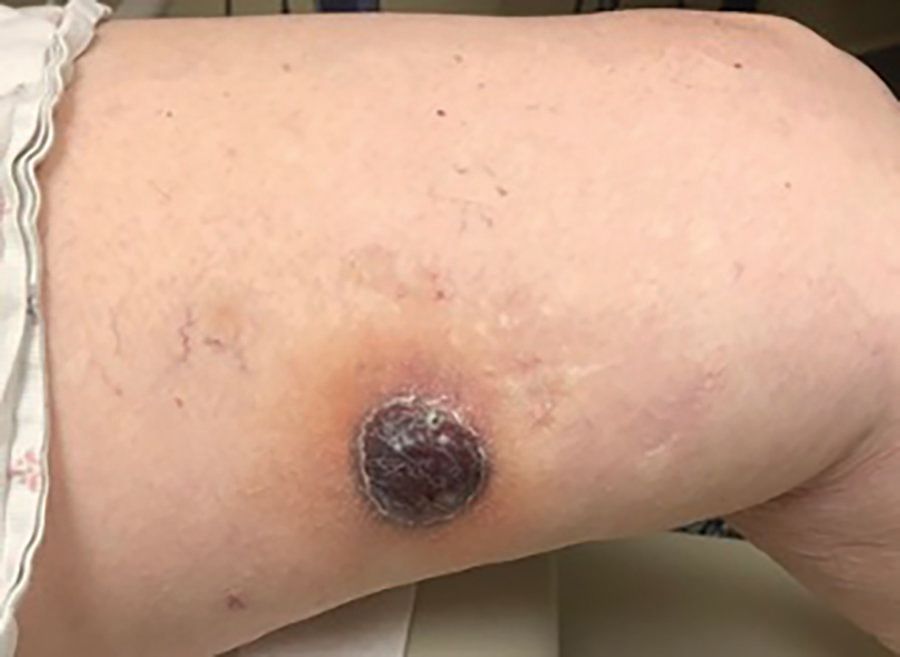
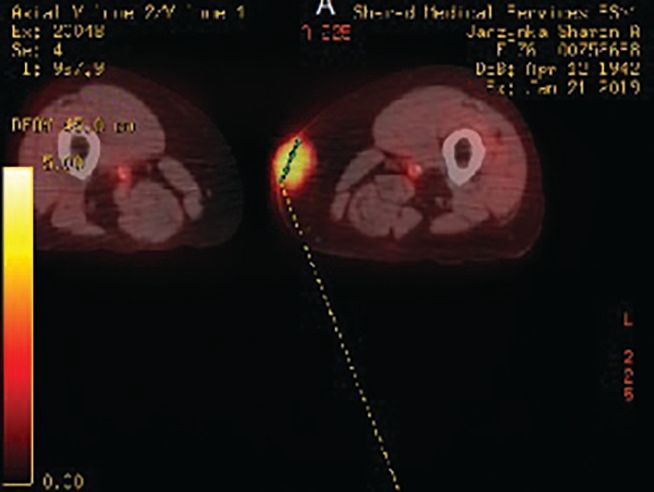
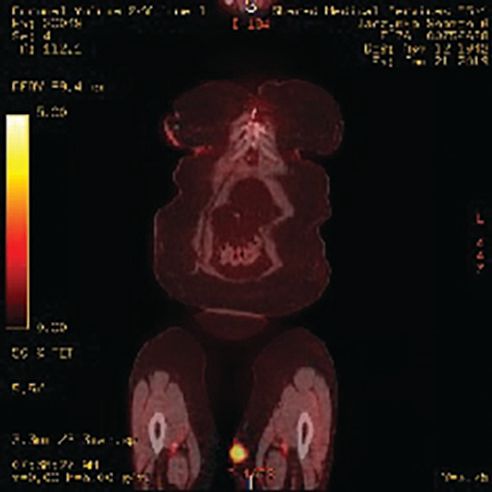
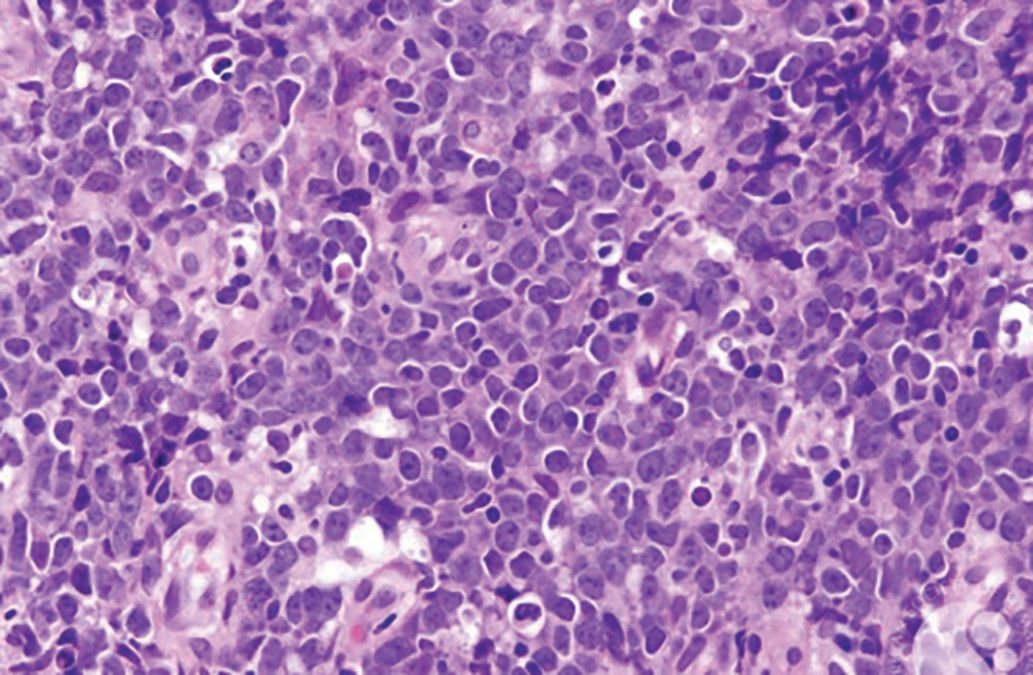
A woman, aged 76 years, presented with a bluish-purple lump in her mid- to upper medial left thigh. It started initially as a flat rash, and over a 2-month period, it turned into a mass measuring 2.5 cm by 3.1 cm (Figure 1). Work-up, including a PET-CT scan, showed the soft tissue mass on the inner thigh to have a Standardized Uptake Value of 4 (Figure 2); there were no other sites of disease. A biopsy of the lesion was performed (Figure 3).
What’s your diagnosis?
A. Kaposi sarcoma
B. Malignant melanoma
C. Adult soft tissue sarcoma
D. Angiosarcoma
E. Lymphoma
CORRECT ANSWER
E. Lymphoma
Comment
Primary cutaneous diffuse large B-cell lymphoma (LBCL), leg type, is a primary cutaneous LBCL of intermediate behavior. It represents 1% to 4% of all cutaneous lymphomas and approximately 10% to 20% of all primary cutaneous LBCLs.1,2 The disease predominantly affects elderly patients, with the male-to-female ratio ranging from 1:2 to 1:4. Typically, patients present with rapidly growing, solitary or clustered, red or bluish-red nodules or tumors located on 1 or both legs, which can ulcerate.3 These lymphomas are mostly limited to the skin at presentation. Histologically, observed is either a dense, diffuse infiltrate of a monotonous population; or confluent sheets of medium to large B cells with round nuclei, prominent nucleoli, and coarse chromatin resembling centroblasts and/or immunoblasts within the dermis and subcutis. The neoplastic B cells usually express B-cell markers (CD19, CD20, CD22, CD79a). Additionally, Bcl-2, MUM1/IRF4, IgM, and FOXP1 proteins are strongly positive.4 The frequent relapses require appropriate treatment decisions and a strict follow-up of the patients.
References:
1. Sokol L, Naghashpour M, Glass LF. Primary cutaneous B-cell lymphomas: recent advances in diagnosis and management. Cancer Control. 2012;19(3):236-244. doi:10.1177/107327481201900308
2. Thomas V, Dobson R, Mennel R. Primary cutaneous large B-cell lymphoma, leg type. Proc (Bayl Univ Med Cent). 2011;24(4):350-353. doi:10.1080/08998289.2011.11928757
3. Kempf W, Denisjuk N, Kerl K, et al. Primary cutaneous B-cell lymphomas. J Dtsch Dermatol Ges. 2012;10(1):12-22; quiz 23. doi:10.1111/j.1610-0387.2011.07852.x
4. Hristov AC. Primary cutaneous diffuse large B-cell lymphoma, leg type: diagnostic considerations. Arch Pathol Lab Med. 2012;136(8):876–881. doi:10.5858/arpa.2012-0195-RA