A Rational Approach to Managing Prostate Cancer in an Irrational Time
The chairman of the Glickman Urological & Kidney Institute at the Cleveland Clinic provides commentary and an adjacent perspective to the Duke Cancer Institute report.
Klein is chairman at Glickman Urological & Kidney Institute Cleveland Clinic

Judd W. Moul, MD and colleagues have nicely outlined the challenges that virtually all developed countries are facing during the onslaught of SARS-CoV-2. Most states have enacted temporary bans against all but essential surgeries; they have left local physicians to use their judgment to determine the meaning of “essential,” considering individual threats to life, limb, and vital organ systems and progression in stage or metastasis for cancers, while ensuring the safety of patients and caregivers with respect to maintaining an adequate supply of intensive care unit (ICU) beds, ventilators, and personal protective equipment (PPE). Thus, in large measure, the definition of “essential” depends on local conditions: the incidence of infection, the capacity of the regional hospital system, the number of affected caregivers who may be temporarily out of the workforce, the daily burn rate of PPE use, and so on.
For the management of cancer in general, there are other factors to consider in deciding what is “essential,” including increased potential exposure to coronavirus infection in immunocompromised patients needing to go to a treatment center for chemo- or immunotherapy; patient anxiety related to delaying initiation of or ongoing therapy; and concerns about whether delaying therapy could influence the chance for cure.
Fortunately for patients with prostate cancer, a substantial amount of evidence from vast experience with active surveillance indicates that those with very low-, low-, and intermediate-risk disease do not compromise their chance for cure by delaying curative treatment.1 Although fewer data are available for those with high-risk (HR) and very high-risk (VHR) disease, in a recently published retrospective pooled analysis from 3 high-volume tertiary centers, we found no difference in rates of biochemical failure, metastasis, prostate-cancer–specific mortality, or all-cause mortality in those with HR or VHR disease treated <8, within 8-12, or >12 weeks after diagnosis.2 In our observation and experience, a delay of up to 90 days for locally advanced or high-grade prostate cancer does not seem to have an adverse effect on short-term outcomes, although 1 prior report found that for HR disease, biochemical failure rates were worse for those with a delay of >90 days.3 An alternative strategy is the use of androgen deprivation therapy as a delaying tactic, which presumably can delay the risk of tumor progression indefinitely. This is also likely safe, at least for a few months, but it’s not clear if the extra cost and toxicity are worth the presumed safety margin, and there is a risk that use for as little as 24 weeks can induce genomic changes characteristic of metastatic castrate-resistant disease, which could compromise cure.4
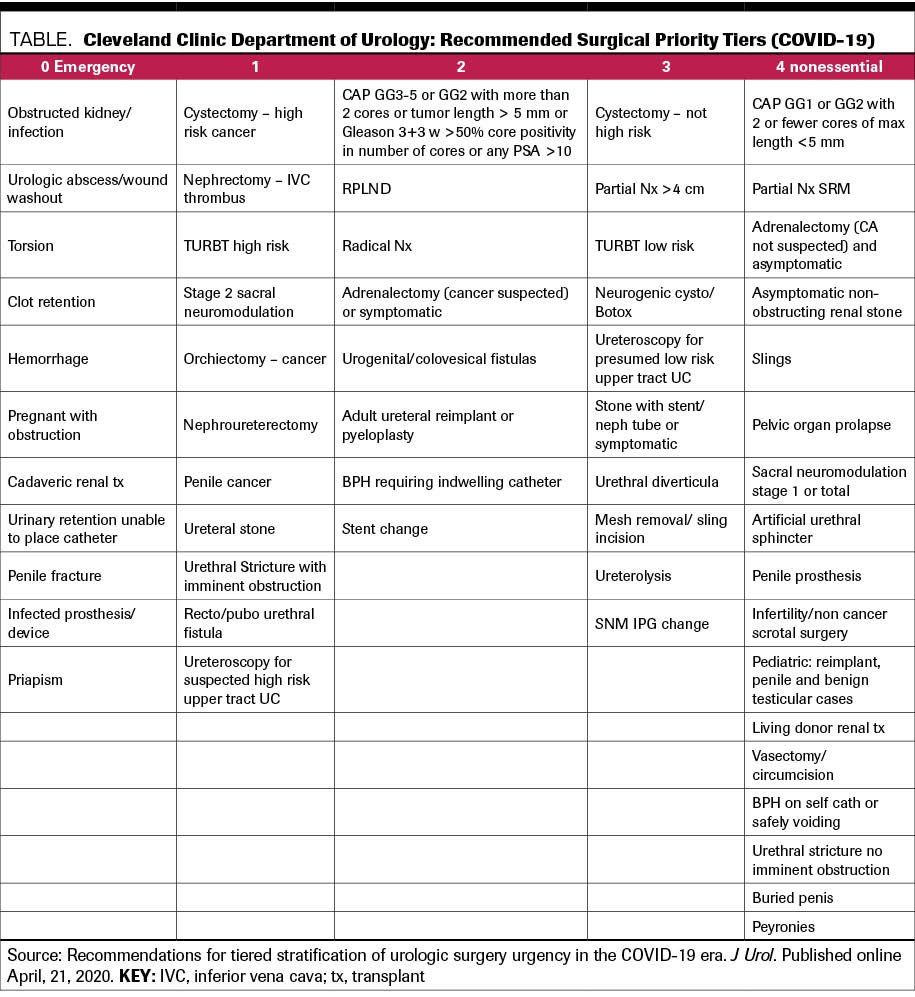
At Cleveland Clinic, we have considered cancer-related and non–cancer-related factors and devised a tiered approach to performing urological surgery and office procedures (Figure).5 At the initial stage of the crisis, when the magnitude of the number and severity of SARS-CoV-2 cases was unknown, we worked with institutional leadership and the decision was made to put all tier 3 and 4 surgeries on hold. As events evolved, and it became clear that early stay-at-home orders and social distancing were effective in flattening the incidence curve in northeast Ohio and that our hospital and caregiver resources would not be overwhelmed with cases, we began (starting the week of April 20) doing tier 3 cases on a limited basis as our system ramps up again, based on availability of operating rooms and nursing and anesthesia personnel, and on patient preference. We have followed a similar process for office-based and nursing procedures. System-wide real-time information with daily monitoring of resources has allowed us to do this safely: The creation of dashboards to monitor system-wide hospitalization and ICU usage for COVID-19-related and non–COVID-19-related care and PPE usage/stock availability, along with our tiered approach to procedures, allows for a rational, measured, and real-time approach that can be dialed back or ramped up as dictated by events related to SARS-CoV-2.
References:
1. Ahmad AE, Richard PO, Leão R, et al. Does time spent on active surveillance adversely affect the pathologic and oncologic outcomes in patients undergoing delayed radical prostatectomy? J Urol. Published online April 7, 2020. doi:10.1097/JU.0000000000001070
2. Reichard CA, Nyame YA, Sundi D, et al. Does time from diagnosis to treatment of high- or very-high-risk prostate cancer affect outcome? BJU Int. 2019;124(2):282-289. doi:10.1111/bju.14671
3. Zanaty M, Alnazari M, Ajib K, et al. Does surgical delay for radical prostatectomy affect biochemical recurrence? a retrospective analysis from a Canadian cohort. World J Urol. 2018;36(1):1-6. doi:10.1007/s00345-017-2105-6
4. Sowalsky AG, Ye H, Bhasin M, et al. Neoadjuvant-intensive androgen deprivation therapy selects for prostate tumor foci with diverse subclonal oncogenic alterations. Cancer Res. 2018;78(16):4716-4730. doi:10.1158/0008-5472.CAN-18-0610.
5. Goldman HB, Haber GP. Recommendations for tiered stratification of urologic surgery urgency in the COVID-19 era. J Urol. Published online April 21, 2020. doi:10.1097/JU.0000000000001067
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.