Around the Practice: Relapsed/Refractory HER2+ Metastatic Breast Cancer
Experts discusses the treatment of patients with HER2-positive breast cancer in a virtual CancerNetwork® Around the Practice presentation,“Relapsed/Refractory HER2+ Metastatic Breast Cancer,” held January 21, 2021, and moderated by Adam M. Brufsky, MD, PhD.
Improvements in extracranial disease control and survival of patients with HER2-positive (+) metastatic breast cancer have led to an increased proportion of patients living long enough to develop central nervous system (CNS) metastases. The recent development of HER2-targeted therapies with CNS activity may improve survival of patients with CNS metastases and prevent development of new CNS metastases. Experts discussed this in a virtual CancerNetwork® Around the Practice presentation, “Relapsed/Refractory HER2+ Metastatic Breast Cancer,” held January 21, 2021, and moderated by Adam M. Brufsky, MD, PhD. The presentation also included an interactive online platform for members of the audience to submit responses to polling questions that were subsequently discussed by the panelists.
Treatment of HER2+ Metastatic Breast Cancer
The standard-of-care therapy in the frontline setting for patients with HER2+ metastatic breast cancer is taxane chemotherapy with the HER2-targeted monoclonal antibodies trastuzumab and pertuzumab. This regimen is based on results from the CLEOPATRA trial (NCT00567190), which showed that treatment with trastuzumab, pertuzumab, and docetaxel led to median progression-free survival (PFS) of 18.7 months and a median overall survival (OS) of 57 months in women with HER2+ metastatic breast cancer.1,2 The HER2-targeted antibody-drug conjugate (ADC) trastuzumab emtansine (T-DM1) is commonly used in the second-line setting. In the EMILIA trial (NCT00829166), it was associated with an OS rate of 30.9 months and median PFS of 9.6 months in patients with locally advanced or metastatic HER2+ metastatic breast cancer previously treated with trastuzumab and a taxane.3 No standard of care has been established for third or later lines of therapy; with current options, the response rate and median PFS are modest (9%-31% and 3-6 months, respectively).4
In clinical practice, docetaxel is often substituted for paclitaxel to provide a treatment option with an alternative dosing schedule, said Neil M. Iyengar, MD. “In our anecdotal experience here, [it is] a little easier to manage adverse events [AEs] with docetaxel,” he said. “As we start to talk about metastatic disease where median PFS continues to be prolonged, a treatment approach that is more manageable in the long term is important.” Docetaxel treatment may be discontinued when the patient achieves treatment response and reinitiated if there is disease progression, or when docetaxel is appropriate in combination with a HER2-targeted antibody. Iyengar noted that this intermittent dosing approach for docetaxel is also a promising area of research for reducing chemotherapy-related AEs and prolonging the period of maintenance antibody-based therapy with a nonchemotherapy partner agent.
V. K. Gadi, MD, PhD, added that with the improvement in long-term outcomes of adjuvant treatment of HER2+ metastatic breast cancer, a greater proportion of metastatic disease presentations are in patients who have not received prior treatment and, thus, are potentially curable (as opposed to presentations in patients who had received prior treatment for early-stage disease and had a metastatic recurrence). “A lot of those patients [with treatment-naïve disease] can get very good, stable, long-term disease control, and, at some point, we might just call that a cure,” said Gadi.
However, Sara A. Hurvitz, MD, cautioned that the identification of patients who can safely discontinue therapy is challenging and requires shared decision-making with the patient. “For some patients, in a shared way, we’ve decided to stop therapy and watch closely and see what happens,” she said. “It really does, given the lack of evidence, need to be a shared decision.”
Management of CNS Metastases in HER2+ Metastatic Breast Cancer
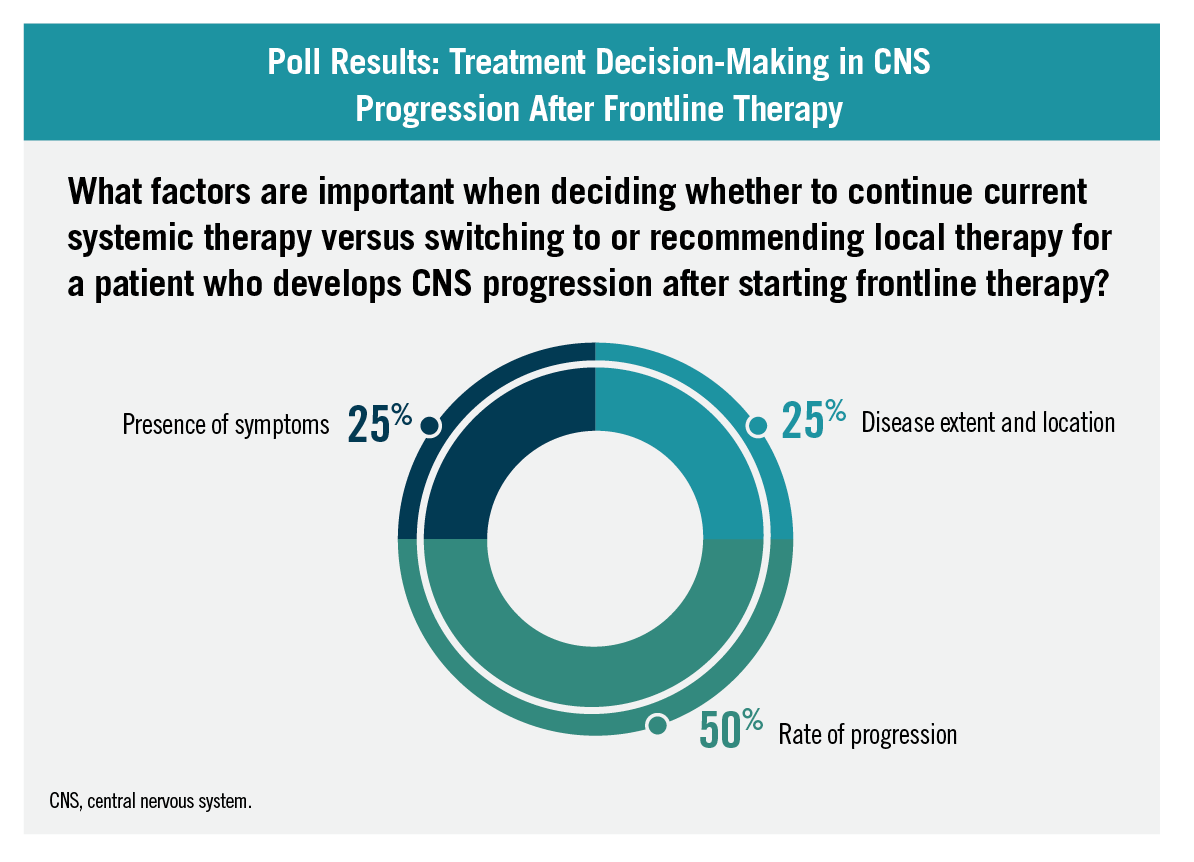
Despite the effective treatment of early-stage disease and extracranial metastases, rates of CNS metastases remain high with HER2+ metastatic breast cancer, occurring in approximately 40% to 50% of patients.5 During the event, 50% of audience members identified that the rate of progression is an important factor when deciding whether to continue current systemic therapy or switch to local therapy for a patient who develops CNS progression after starting frontline therapy. Other answer choices that received responses included disease extent and location (25%) and presence of symptoms (25%).
Poll Results: Treatment Decision-Making in CNS Progression After Frontline Therapy
For patients with CNS metastases, stereotactic radiosurgery (SRS) has the potential to provide durable therapeutic responses and is a preferred therapeutic option. SRS delivers photon radiation with high precision compared with whole-brain radiation. Whole-brain radiation is associated with cognitive function AEs and impairments in quality-of-life outcomes. Despite the benefits of SRS, it is also associated with a high rate of neurologic complications, which can vary.6 Despite the benefits of SRS, it is also associated with a high rate of neurologic complications, which can vary based on the involved brain regions.6 Surgical resection may also be considered for patients with limited sites of disease that are surgically accessible and within a reasonable functional status.6
Local therapy is generally indicated for patients whose disease has adequate systemic control, thus highlighting a need for systemic-based therapies for patients who also have extracranial metastases.6
Gadi said that a multidisciplinary approach, crafted with input from a neuroradiation oncologist and possibly a neurooncologist, is important for optimal management of patients with CNS metastases. Patient symptoms should guide the management approach, he added. “If a patient has symptoms, then you need to address the symptoms,” he said. “If the patient doesn’t have symptoms or it’s an incidental finding or something that could be managed with SRS, that becomes a viable option as well.”
Gadi added that tucatinib is also a promising option in this setting for some patients, based on recent data from the phase 3 HER2CLIMB trial (NCT02614794). The results showed that, compared with placebo, tucatinib added to trastuzumab and capecitabine led to a 68% reduction in risk for brain progression and death, as well as a 42% reduction in risk of death in patients with HER2+ metastatic breast cancer that had metastasized to the brain and had been treated previously with trastuzumab, pertuzumab, and T-DM1.7 The median duration of PFS in the CNS was 9.9 months in the tucatinib arm and 4.2 months in the placebo arm; estimated OS at 1 year was 70.1% and 46.7% in the tucatinib and placebo arms, respectively.7
“I think [decisions must] still [be made on] a case-by-case basis, but it gives us a pretty powerful tool to proactively manage the CNS metastasis with or without SRS,” said Gadi.
However, whether tucatinib should be used before or instead of SRS is currently unclear and likely depends on the number of metastases in the brain, according to Iyengar. “If it’s a question about something like SRS to a single lesion, my preference and the preference of our neuroradiation oncologist is generally to proceed with SRS to the single lesion,” Iyengar said. “If we’re talking about more diffuse, maybe multiple parenchymal metastases, and the question is whole brain versus something like tucatinib, I think that’s more of a discussion. We tend to err on the side of local therapy, followed by perhaps a switch of [the] systemic therapy [regimen] until we see more data for that cohort of untreated brain metastases population.”
With PFS and OS consistently lower in patients with brain metastases, figuring out optimal sequences of locoregional and systemic therapy continues to be important, according to Hurvitz. She pointed out that patients in the HER2CLIMB study who had a CNS progression on trial were allowed to receive SRS or radiation therapy and to continue in the trial if they did not have extracranial progression. “We can do that in clinical practice where patients are started on tucatinib-based therapy, and if they have an isolated CNS progression, you have data to support treating it locoregionally and continuing systemic therapy,” she said.
Although tucatinib is the only approved agent for metastatic HER2+ metastatic breast cancer and the only one that has demonstrated substantial response in the brain, some data suggest that certain HER2-targeted therapies may delay time to initial development of brain metastases. Results of the NEfERT-T trial (NCT00915018) of patients with treatment-naïve, HER2+ metastatic breast cancer showed that neratinib and trastuzumab had a similar objective response rate and duration of response when added to paclitaxel, but the neratinib regimen was associated with significantly lower estimated Kaplan-Meier 2-year incidence of CNS recurrences (16.3% vs 31.2%; P = .004).8
Gadi also noted the possibility of T-DM1 delaying the onset of CNS metastases, although the ADC’s large molecular size was traditionally thought to preclude CNS access. “If you have a drug that is very, very good at maintaining systemic disease at a low level…then you would interpret that as an effect in the brain,” said Gadi. “But now I think there’s some emerging evidence that these molecules are actually crossing the blood-brain barrier. They’re detectable in the CNS, and maybe they are actually [reaching the brain] in enough quantity to impart an effect directly on brain metastases.”
Case 1: The panelists discussed their approach to management of the case of a woman, age 48 years, with HER2+ metastatic breast cancer, 3 lesions in the liver, and no CNS metastases at initial presentation. She received 6 cycles of docetaxel, trastuzumab, and pertuzumab, followed by trastuzumab and pertuzumab for an additional 12 months, to which the breast lesion had a partial response and the liver lesions had a full response. Then, she developed 2 new liver lesions and approximately 30 small lesions scattered throughout the brain.
Case 1 Discussion
Half of the audience revealed that 50% of respondents recommended tucatinib, trastuzumab, and capecitabine for this patient and the other 50% recommended SRS to the brain metastases.
CASE 1: What treatment would you recommend for this patient?
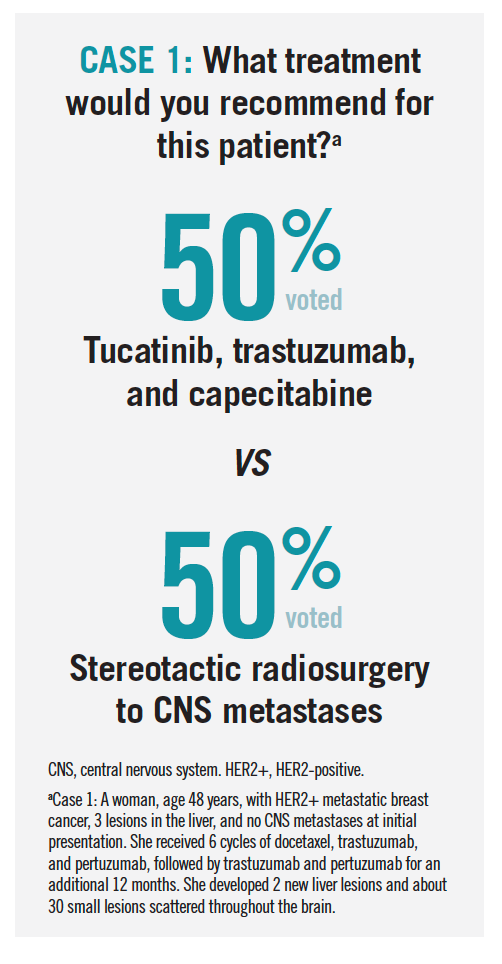
Hurvitz pointed out that SRS and switching systemic therapy should be considered because of the systemic progression in the liver in addition to new-onset brain metastases. “I like tucatinib because it does penetrate the blood-brain barrier, but probably would talk to my radiation oncology and neurosurgery colleagues,” she said. “I’m thinking we’d probably end up doing both the SRS and tucatinib-based therapy.”
Iyengar added that the relatively good tolerability of the tucatinib-based regimen makes it a reasonable option and that although diarrhea is a common AE, it usually improves or resolves with initiation of antidiarrheal agents. He also noted that many of the AEs with the regimen are likely related to capecitabine, and most practices are experienced with managing these and modifying the dose as necessary.
Gadi concluded that it is important to continue to assess the data on patient-reported outcomes from the studies of tucatinib with capecitabine, as the regimen’s high pill burden may negatively affect patient quality of life. “From our perspective as physicians, yeah, this is a slam dunk, it’s easy to give. But that’s not the perspective that matters sometimes,” he pointed out.
Treatment After Progression on More Than 2 Prior Lines of Anti-HER2 Targeted Therapy
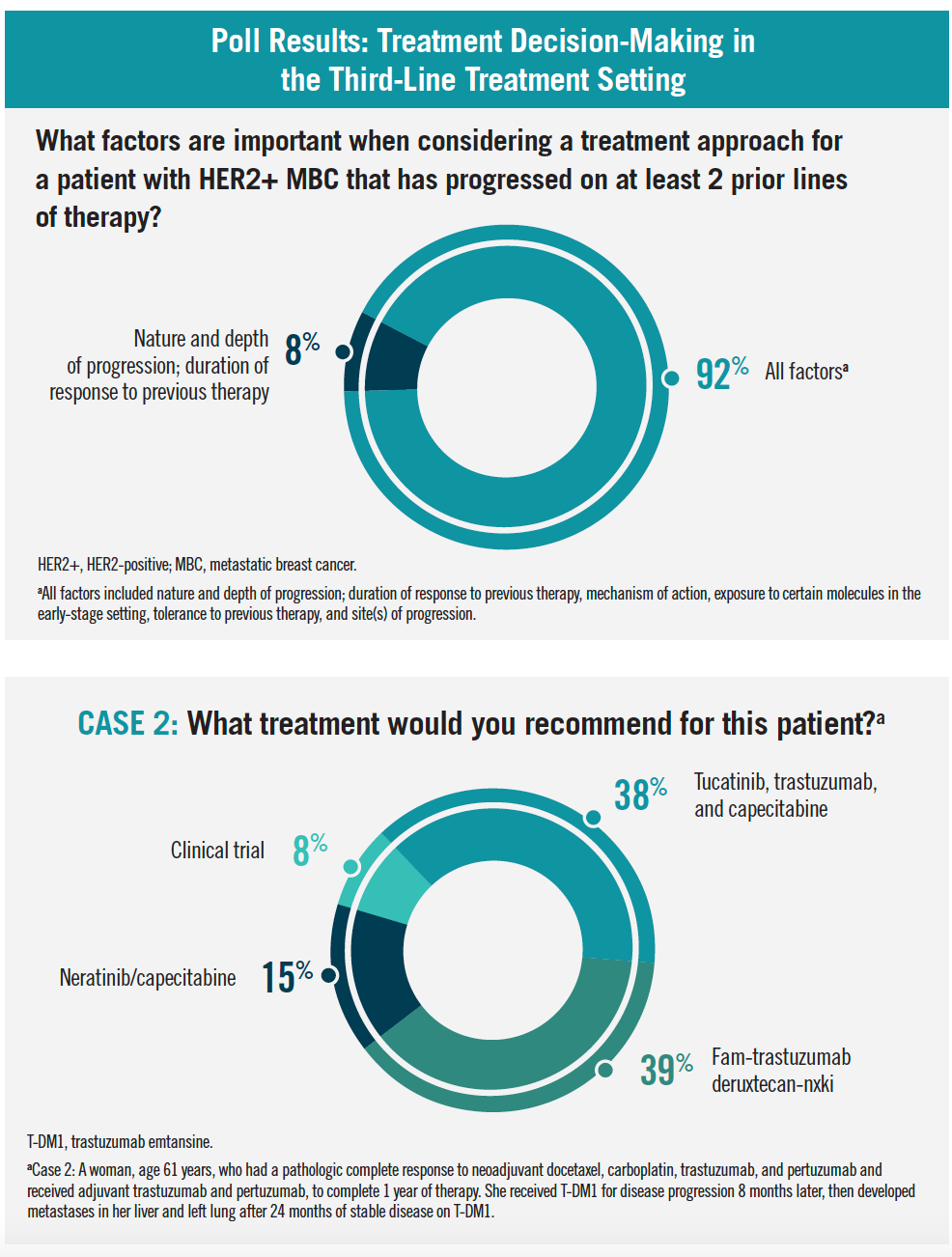
In a poll of the audience, 92% of respondents stated that selection of a treatment approach for a patient with HER2+ metastatic breast cancer who has progressed on 2 or more prior lines of therapy should consider all the listed factors (ie, nature and depth of progression, duration of response to previous therapy, mechanism of action and exposure to certain molecules in the early-stage setting, tolerance to previous therapy, site[s] of progression), whereas the remaining 8% selected nature and depth of progression plus duration of response to previous therapy as the primary factors to consider.
Hurvitz said that she does not use neratinib frequently in her practice because the toxicity profile is difficult for patients to manage. “We don’t have evidence that neratinib works well after tucatinib, which is where I would place it,” she said. “We need evidence of whether or not neratinib works in brain metastases and in systemic metastases, post tucatinib. If it does, that’s probably where I’ll use it.”
Hurvitz said that, in contrast, she is a “big fan” of trastuzumab deruxtecan (DS-8201), an ADC consisting of a humanized HER2-targeted monoclonal antibody with the same amino acid sequence as trastuzumab, a cleavable tetrapeptide-based linker, and a potent topoisomerase I inhibitor as the cytotoxic drug (ie, payload).4 Trastuzumab deruxtecan also has a higher drug-to-antibody ratio than T-DM1 (approximately 8:1 vs 3-4:1) while maintaining a favorable pharmacokinetic profile.4 Results of the phase 2 DESTINY-Breast01 trial (NCT03248492) showed a response rate of 60.9%, median PFS duration of 16.4 months, and estimated 12-month OS rate of 86.2% in patients with heavily pretreated metastatic HER2+ metastatic breast cancer who had a median of 6 prior lines of therapy for
metastatic disease.4
Hurvitz cautioned that treatment-related interstitial lung disease (ILD), which was reported in 13.6% of patients in the DESTINY-Breast01 trial, can mimic lung disease induced by COVID-19; Iyengar added that the drug-related ILD can progress rapidly, and the risk of ILD needs to be weighed against the potential benefit in treatment response.4 Iyengar added that he orders baseline pulmonary function testing to assess the patient’s function prior to starting the drug. Assessing for history of prior lung disease and risk for Coronavirus 2019–related lung disease is important prior to starting trastuzumab deruxtecan, he noted.
Poll Results: Treatment Decision-Making in the Third-Line Treatment Setting
Case 2: The panelists discussed treatment options for the case of a woman, age 61 years, who had a pathologic complete response to neoadjuvant docetaxel, carboplatin, trastuzumab, and pertuzumab and received adjuvant trastuzumab and pertuzumab, and completed 1 year of therapy. She received T-DM1 for disease progression 8 months later, then developed metastases in her liver and left lung after 24 months of stable disease on T-DM1.
Case 2 Discussion
An audience poll revealed that an equal number of clinicians would recommend tucatinib, trastuzumab, and capecitabine or trastuzumab deruxtecan (38%); 15% would recommend neratinib plus capecitabine; and 8% would recommend a clinical trial.
Hurvitz said that she favors tucatinib in this scenario even though the patient does not have brain metastases, given its reasonably good tolerability and the randomized data that support its efficacy. “We don’t yet have randomized data supporting the use of trastuzumab deruxtecan, so I like the tucatinib idea, hoping that maybe it will postpone or mitigate the risk of progression in the brain,” she said.
Similarly, Gadi said that he favors tucatinib in this case, given its robust evidence, but he noted, “I don’t fault anybody for picking the deruxtecan here because it is such an active agent in somebody with rapid progression.”
The ongoing phase 3 DESTINY-Breast03 trial (NCT03529110), which is comparing trastuzumab deruxtecan with T-DM1 in patients with metastatic HER2+ metastatic breast cancer previously treated with trastuzumab and taxane chemotherapy, will provide randomized data regarding the efficacy and safety of trastuzumab deruxtecan and has an estimated completion date of April 2023.9 However, Gadi said that he is unlikely to preferentially use it over tucatinib, given the potential toxicities associated with trastuzumab deruxtecan, although having both drugs to sequence will be beneficial. “The one other concern I have with deruxtecan is whether patients will be fit to try another line of therapy after it,” he said. “If we know the drug is going to work after other stuff has worked, I might try the other stuff first and then have this available to me in that third-line setting.” However, all the panelists agreed that although they would prefer tucatinib, either tucatinib or trastuzumab deruxtecan is appropriate in this setting, provided the patient is healthy enough from a pulmonary standpoint.
REFERENCES
1. Swain SM, Baselga J, Kim SB, et al; CLEOPATRA Study Group. Pertuzumab, trastuzumab, and docetaxel in HER2-positive metastatic breast cancer. N Engl J Med. 2015;372(8):724-734. doi:10.1056/NEJMoa1413513
2. Swain SM, Miles D, Kim S-B, et al. End-of-study analysis from the phase III, randomized, double-blind, placebo (Pla)-controlled CLEOPATRA study of first-line (1L) pertuzumab (P), trastuzumab (H), and docetaxel (D) in patients (pts) with HER2-positive metastatic breast cancer (MBC). J Clin Oncol. 2019;37(suppl 15):1020. doi:10.1200/JCO.2019.37.15_suppl.1020
3. Verma S, Miles D, Gianni L, et al; EMILIA Study Group. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783-1791. doi:10.1056/NEJMoa1209124.
4. Modi S, Saura C, Yamashita T, et al; DESTINY-Breast01 Investigators. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer. N Engl J Med. 2020;382(7):610-621. doi:10.1056/NEJMoa1914510
5. Wu Q, Liao W, Zhang M, Huang J, Zhang P, Li Q. Cost-effectiveness of tucatinib in human epidermal growth factor receptor 2–positive metastatic breast cancer from the US and Chinese perspectives. Front Oncol. 2020;10:1336. doi:10.3389/fonc.2020.01336
6. Nasrazadani A, Brufsky A. Neratinib: the emergence of a new player in the management of HER2+ breast cancer brain metastasis. Future Oncol. 2020;16(7):247-254. doi:10.2217/fon-2019-0719
7. Lin NU, Borges V, Anders C, et al. Intracranial efficacy and survival with tucatinib plus trastuzumab and capecitabine for previously treated HER2-positive breast cancer with brain metastases in the HER2CLIMB trial. J Clin Oncol. 2020;38(23):2610-2619. doi:10.1200/JCO.20.00775
8. Awada A, Colomer R, Inoue K, et al. Neratinib plus paclitaxel vs trastuzumab plus paclitaxel in previously untreated metastatic ERBB2-positive breast cancer: the NEfERT-T randomized clinical trial. JAMA Oncol. 2016;2(12):1557-1564. doi:10.1001/jamaoncol.2016.0237
9. DS-8201a versus T-DM1 for human epidermal growth factor receptor 2 (HER2)-positive, unresectable and/or metastatic breast cancer previously treated with trastuzumab and taxane [DESTINY-Breast03]. ClinicalTrials.gov. Updated December 4, 2020. Accessed February 7, 2021. https://www.clinicaltrials.gov/ct2/show/NCT03529110#wrapper