Burnout in Oncology
Burnout is defined as an occupational-related syndrome characterized by physical and emotional exhaustion, cynicism/depersonalization, and low sense of professional accomplishment.

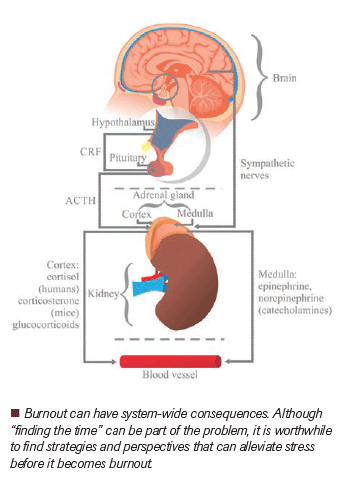
ABSTRACT: Burnout is defined as an occupational-related syndrome characterized by physical and emotional exhaustion, cynicism/depersonalization, and low sense of professional accomplishment. Multiple oncology-specific risk factors are associated with an increased susceptibility for the development of burnout. On a daily basis, oncologists are faced with life and death decisions and grieving much more frequently than are physicians in other specialties. Continuous exposure to fatal illnesses with limited success in curing them, exceedingly long work hours with more administrative time demands, limited autonomy over daily responsibilities, endless electronic documentation requirements, and a shifting medical landscape seem to be making oncologists more vulnerable to suffering from burnout. Evidence suggests that burnout can impact quality of care in a variety of ways and have potentially profound personal implications. In this review, the definition, prevalence, causes, and management of oncologist burnout are analyzed. Steps oncologists can take to promote personal well-being and professional satisfaction are also explored.
Introduction
Oncology is largely viewed as an inherently challenging specialty due to its nature of dealing with daily life and death circumstances. Exposure to long hours of direct patient care for desperately ill patients, counseling their families, endless electronic documentation requirements, continual loss of autonomy over daily responsibilities, and a constantly changing medical environment set the stage for what is called a “burnout syndrome” for most practicing oncologists. Feeling inadequately equipped to deal with the emotional reactions of patients and their families can be a further source of stress among oncologists whose daily work may also force them to face their own mortality, as well as that of their family and friends.
Burnout was first described by psychologist Herbert Freudenberger in the 1970s as a condition that occurs when work coupled with additional life pressures exceeds the ability to cope, resulting in physical and mental distress.[1] In the 1980s came the 22-item Maslach Burnout Inventory (MBI)–Human Services Survey, which became the most widely used and validated assessment tool for self-reported symptoms of burnout.[2] The MBI consists of three distinct components: emotional exhaustion, depersonalization, and personal accomplishment/experience of ineffectiveness. These components, however, are usually part of a continuum that may include overlapping symptoms of cardiovascular, gastrointestinal, musculoskeletal, cognitive, and affective origin. The Copenhagen Burnout Inventory, which was introduced in the early 2000s, gauges burnout at three scales: personal burnout, work-related burnout, and client-related burnout.[3] Finally in May 2019, the World Health Organization added burnout to the 11th revision of the International Classification of Diseases (ICD-11), characterizing it as a syndrome of three dimensions: feelings of energy depletion or exhaustion, increased mental distance from one’s job or feelings of cynicism or negativism about one’s job, and reduced professional efficacy.[4]
Energy depletion or exhaustion is described as a complete lack of energy frequently resulting in a debilitating feeling of dread for what the day ahead will bring. Basic tasks and, sadly, even things that would normally provide joy turn into chores. Trouble sleeping to the point of insomnia, inability to rest and recharge, and difficulty to concentrate and focus eventually lead to panic attacks, chest pain, breathing difficulties, migraines, and stomach pains. Increased mental distance from one’s job and feelings of cynicism or negativism about that job refer to feelings of worthlessness, hopelessness, and an inability to accept consolation or connect to the empathy offered by others, leading to isolation from work, family, friends, and life. Reduced professional efficacy can manifest as going through the motions, making it to the office, and somehow still getting the job done in an almost robotic manner. There is no zest, no pleasure, and therefore, no optimum performance. Ordinary tasks take longer, and things that were once easy now seem overwhelming.
Burnout is not a diagnosis listed in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, but it is classified by ICD-11 as a phenomenon under problems associated with employment and has been recognized as a diagnosable condition (diagnostic code QD85) resulting from chronic workplace stress about exhaustion, cynicism, and reduced efficacy. Notably, it is highlighted to be an occupational phenomenon rather than a medical condition. [4] An occupational phenomenon is defined as factors influencing health status or contact with health services, which includes reasons individuals look for health services. It is not classified as an illness or health condition.
The hallmark features of burnout are similar to the criteria for endogenous depression; however, ICD-11 specifically excludes mood disorders from the definition of burnout. Although burnout is classified and conceptualized as a workplace-related disorder, this assertion may not be entirely true. Burnout may look similar to depression and other psychiatric disorders, in that it is multifactorial and complex. Symptoms of emotional exhaustion and depersonalization can originate from not only direct workplace stress but also stress at home, such as having difficulties in marriage, having to care for an older parent, or a long commute to work, and more. Many of the factors that contribute to depression also contribute to burnout. Sufficiently long vacations can help differentiate depression from burnout, but burnout relief post vacation has been shown to be short lived. [5] Psychiatrists who support physicians affected by burnout are left to consider the possibility of differential diagnoses or comorbidities because burnout and depression may have overlapping symptoms and clinical features. The stigma of mental illness and its treatment may allow burnout to become a catchall term for emotional distress and thus less stigmatized. Importantly, erroneously labeling a physician’s distress as burnout may prevent or delay appropriate treatment of depression and sometimes a life-threatening mental disorder.
As burnout is poorly defined, one may expect considerable variation in the reported prevalence of burnout to exist due to significant differences in the way it has been defined, diagnosed, and assessed. [6, 7] Depending on the definition chosen, the prevalence of burnout identified can vary significantly. This complexity arises because the classic triad of burnout symptoms can manifest to differing degrees in each individual. Most of the reported data come from survey studies. A national survey among US oncologists found a 45% burnout prevalence, while other studies reported 20% to 70% burnout rate globally. [8–12] A systematic review and meta-analysis of 4,876 participants from 17 studies reported a 32% rate of burnout, which possibly gives the best estimate on oncologist burnout. [13]
Causes and Risk Factors
Similar to its definition and prevalence, leading causes and risk factors of burnout come from observational, cross-sectional, and survey-type studies. The three most commonly stated causative factors include clinical and nonclinical work burden, electronic medical record (EMR) implementation, and loss of autonomy. Causes and risk factors can be summarized into demographic, workplace, and work/life balance categories. Among demographic factors, younger age, living alone, lack of access to support services, and being an early career oncologist have been found to be related to burnout.[14,15] Workplace-related factors refer to not only increased work hours but also to increased administrative workload and reduced meaningful professional activity such as research and educational time.[16–19] The significant loss of physician independence, excessive time spent on regulatory and clerical work, and stressful professional experiences in delivering bad news to cancer patients have been connected to workplace-related burnout among oncologists.[20–22] Impaired work/life balance occurs when quality time away from work such as vacation time, time for hobbies, and time for family becomes increasingly inadequate.[23,24] Every additional after-hours time at home spent on work-related tasks such as accessing work-related emails and EMRs has been associated with higher rates of burnout.[25]
Managing Burnout in Oncology
As oncologists, we deal with life and death and grieving much more frequently than other specialties. With continuous exposure to lethal illnesses and limited success in curing them, oncologists may seem to be particularly vulnerable to stress and burnout. Challenges of staying ahead of the extensive new discoveries in cancer science and trying to assimilate enormous quantities of new research on new drugs and molecular therapies, augmented by demands posed by EMRs and compliance, regulation, and payment issues, oncologists may very quickly reach a breaking point. Despite speculation that oncologists may be at greater risk for burnout than physicians in other disciplines, however, there have been very few well-designed studies examining distress rates among oncologists relative to other specialties. [26] A preliminary analysis from a national study conducted in collaboration with the American Medical Association of 7,000 US physicians did not find evidence to support the supposition that oncologists are at higher risk for burnout (unpublished data). Medical oncologists (n = 87) had a lower rate of burnout than other internal medicine physicians (n = 1,328), with a burnout rate of 37.9% vs 48.8%, respectively (P = .05). Medical oncologists were also more likely to state they would choose the same specialty if they could redo their career choice compared with other internal medicine physicians, at 81.4% vs 61.9%, respectively (P < .001).[27]
On the brighter side, practicing oncologists caring for cancer patients have the most rewarding profession. Cancer research is intellectually more than stimulating. Witnessing revolutionary discoveries in molecular biology and seeing them translated into clinical practice, ie, “bench to bedside” happening more frequently than in any other specialty, is extremely gratifying. Being part of cancer science discoveries and having the opportunity to implement these advances into clinical practice by taking part in standard care and/or participating in clinical trials, oncologists have the unique advantage of professional satisfaction more than those in other specialties of medicine. Being part of the efforts leading to improved patient outcomes in prevention, diagnosis, treatment, palliative care, and quality of life of cancer patients provides tremendous opportunity for meaning and purpose in the professional lives of oncologists. They can derive high levels of satisfaction from their professional status and associated collegial respect, as well as from the intellectual stimulation that their role provides. [22]
As oncologists, we evaluate and diagnose complex problems, devise and administer individualized treatment strategies, and provide critical support to patients and their families who face life-threatening illnesses. We can identify values and determine how to align our work activities with the areas we find most meaningful. Our relationships with patients, along with the intellectual stimulation that our specialty provides, establish the foundation for professional meaning for many of us. Every day, we directly and indirectly affect hundreds of people’s lives. Although in most other medical specialties beneficence and altruism overlap, in oncology, we have the advantage and capability of being more altruistic than beneficent in our daily practice. In fact, neurobiologists have found that when engaged in an altruistic act, the pleasure centers of the brain become active. [28]
Given the high prevalence of physician distress and the potential repercussions for quality of care, however, hospitals, practice groups, national societies, and healthcare organizations must have a responsibility and obligation in coming up with solutions to help reduce physician burnout. This will require various individual strategies as well as concerted efforts across national, organizational, and departmental levels for change. Professional bodies such as the American Society of Clinical Oncology, the European Society for Medical Oncology, and the Society of Gynecologic Oncology have already taken important steps to promote cultural change through the introduction of sessions addressing burnout at international congresses and the provision of policy recommendations. We oncologists, just like our cancer patients, are strong, resilient, and capable of handling the very demanding aspects of our profession. Still, what is most needed are concerted efforts to address characteristics in the organizational culture and environment that contribute to distress and burnout. These include nonclinical work burden; EMR burden; compliance, regulation, and payment issues; loss of autonomy; productivity-driven staffing models; inefficient use of physician time; and a focus on short-term profitability objectives. [29]
Conclusion
Oncologist burnout is a multifaceted issue with a negative impact on physicians, patients, and institutions. Globally, a multitude of professional bodies and organizational leaders are giving this important subject much-deserved attention. Reducing oncologist burnout will require various individual strategies as well as a concerted effort across national, organizational, and departmental levels for change.
FIVE KEY REFERENCES
4. ICD-11 for Mortality and Morbidity Statistics, QD85 Burn-out. International Classification of Disease, 11th ed. 2019. Available at: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281. Accessed October 29, 2019.
5. de Bloom J, Geurts SAE, Taris TW, et al. Effects of vacation from work on health and well-being: lots of fun, quickly gone. Work Stress. 2010;24:196-216.
9. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678-86.
15. Banerjee S, Califano R, Corral J, et al. Professional burnout in European young oncologists: results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol. 2017;28:1590-6.
29. Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med. 2007;22:1544-52.
References:
1. Freudenberger HJ. Staff burn-out. J Soc Issues. 1974; 30:159-65.
2. Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
3. National Academy of Medicine. Validated instruments to assess work-related dimensions of well-being. Available at: https://nam.edu/valid-reliable-survey-instruments-measure-burnout-well-work-related-dimensions/. Accessed October 29, 2019.
4. ICD-11 for Mortality and Morbidity Statistics, QD85 Burn-out. International Classification of Disease, 11th ed. 2019. Available at: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281. Accessed October 29, 2019.
5. de Bloom J, Geurts SAE, Taris TW, et al. Effects of vacation from work on health and well-being: lots of fun, quickly gone. Work Stress. 2010;24:196-216.
6. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen Burnout Inventory: a new tool for the assessment of burnout. Work Stress. 2005;19:192-207.
7. Legassie J, Zibrowski EM, Goldszmidt MA. Measuring resident well-being: impostorism and burnout syndrome in residency. J Gen Intern Med. 2008;23:1090-4.
8. Schaufeli WB, Bakker AB, Hoogduin K, Schaap C, Kladler A. On the clinical validity of the Maslach Burnout Inventory and the Burnout Measure. Psychol Health. 2001;16:565-82.
9. Shanafelt TD, Gradishar WJ, Kosty M, et al. Burnout and career satisfaction among US oncologists. J Clin Oncol. 2014;32:678-86.
10. Mampuya WA, Matsuo Y, Nakamura A, Hiraoka M. Evaluation of the prevalence of burnout and psychological morbidity among radiation oncologist members of the Kyoto Radiation Oncology Study Group (KROSG). J Radiat Res. 2017;58:217-24.
11. Leung J, Rioseco P, Munro P. Stress, satisfaction and burnout amongst Australian and New Zealand radiation oncologists. J Med Imaging Radiat Oncol. 2015;59:115-24.
12. Mordant P, Deneuve S, Rivera C, et al; European Society of Surgical Oncology Young Surgeons and Alumni Club (EYSAC). Quality of life of surgical oncology residents and fellows across Europe. J Surg Educ. 2014;71:222-8.
13. Medisauskaite A, Kamau C. Prevalence of oncologists in distress: systematic review and meta-analysis. Psychooncology. 2017;26:1732-40.
14. Shanafelt TD, Raymond M, Horn L, et al. Oncology fellows’ career plans, expectations, and well-being: do fellows know what they are getting into? J Clin Oncol. 2014;32:2991-7.
15. Banerjee S, Califano R, Corral J, et al. Professional burnout in European young oncologists: results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol. 2017;28:1590-6.
16. Allegra CJ, Hall R, Yothers G. Prevalence of burnout in the U.S. oncology community: results of a 2003 survey. J Oncol Pract. 2005;1:140-7.
17. Elit L, Trim K, Mand-Bains IH, et al; Society of Gynecologic Oncology Canada. Job satisfaction, stress, and burnout among Canadian gynecologic oncologists. Gynecol Oncol. 2004;94:134-9 .
18. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-21.
19. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016;165:753-60.
20. Landon BE, Reschovsky J, Blumenthal D. Changes in career satisfaction among primary care and specialist physicians, 1997-2001. JAMA. 2003;289:442-9.
21. Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. JAMA. 2017;317:901-2.
22. Ramirez AJ, Graham J, Richards MA, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263-9.
23. Banerjee S, Califano R, Corral J, et al. Professional burnout in European young oncologists: results of the European Society for Medical Oncology (ESMO) Young Oncologists Committee Burnout Survey. Ann Oncol. 2017;28:1590-6.
24. Glasberg J, Horiuti L, Novais M, et al. Prevalence of the burnout syndrome among Brazilian medical oncologists. Rev Assoc Med Bras. 2007;53:85-9.
25. Dhande M. Writing out loud: to computers, patients, and burnout, 2016. JAMA Cardiol. 2016;1:639.
26. Ramirez AJ, Graham J, Richards MA, Cull A, Gregory WM. Mental health of hospital consultants: the effects of stress and satisfaction at work. Lancet. 1996;347:724-8.
27. Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol. 2012;30:1235-41.
28. Klimecki OM, Leiberg S, Ricard M, Singer T. Differential pattern of functional brain plasticity after compassion and empathy training. Soc Cogn Affect Neurosci. 2014;9:873-9.
29. Dunn PM, Arnetz BB, Christensen JF, Homer L. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med. 2007;22:1544-52.
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.