The Role of the Comprehensive Geriatric Assessment in the Evaluation of the Older Cancer Patient
Geriatric assessments have now been recommended as part of the standard evaluation of an older adult considering cancer therapy.

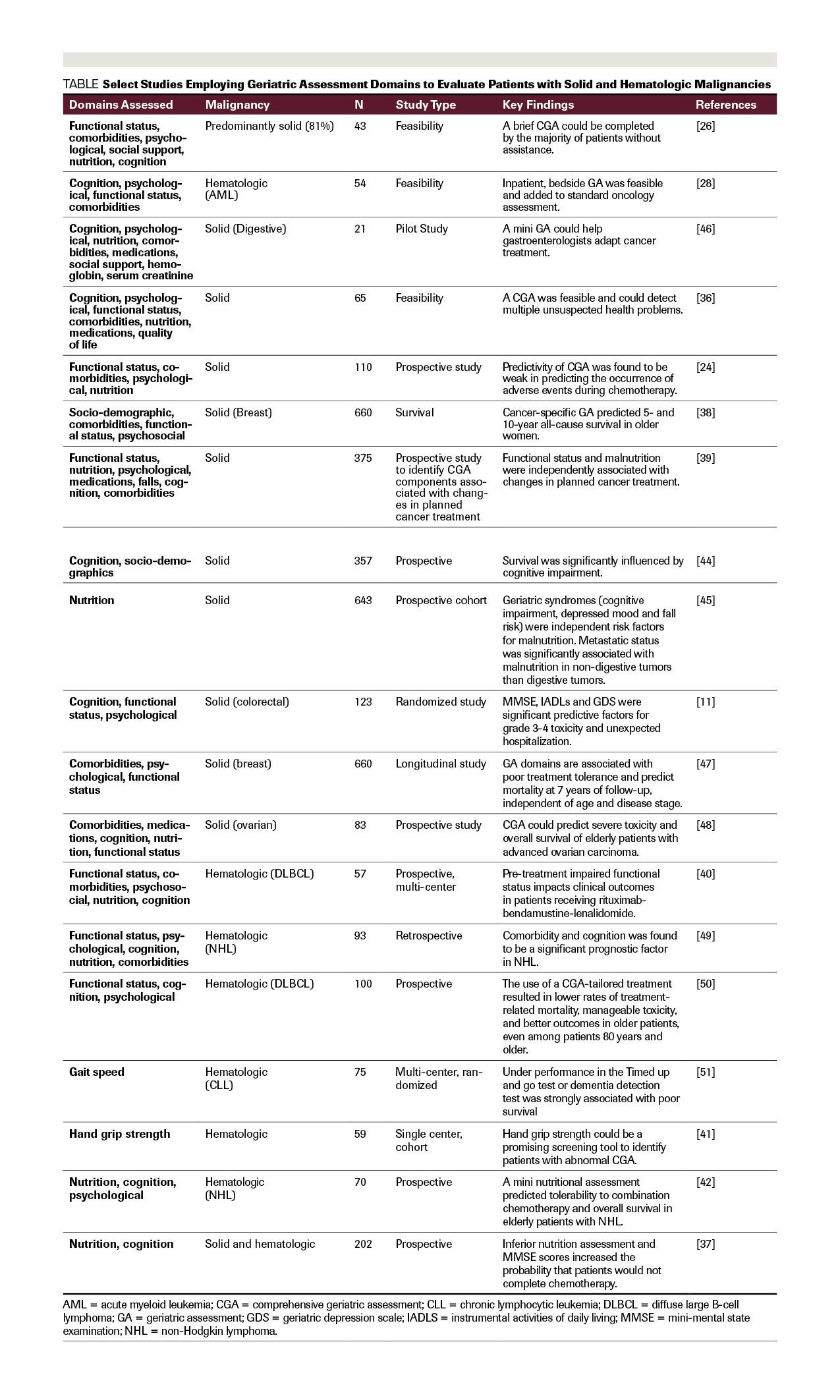
TABLE Select Studies Employing Geriatric Assessment Domains to Evaluate Patients with Solid and Hematologic Malignancies
Dr. Blanquicett is a Medical Oncology/ Hematology Fellow at Moffitt Cancer Center, Tampa, Florida, and is Assistant Professor of Medicine at Emory University in Atlanta, Georgia.

Dr. Johnson is Professor and Chair of General Medicine and Geriatrics in the Department of Family and Preventive Medicine, Emory University School of Medicine, Atlanta, Georgia.

Dr. Flowers is Professor in the Department of Hematology & Medical Oncology, and Co- Director of the Winship Cancer Center Lymphoma Program, Emory University School of Medicine, Atlanta, Georgia.

Dr. Cohen is Associate Professor in the Department of Hematology & Medical Oncology, and Co-Director of the Winship Cancer Center Lymphoma Program, Emory University School of Medicine, Atlanta, Georgia.

ABSTRACT: Geriatric assessments have now been recommended as part of the standard evaluation of an older adult considering cancer therapy. While the need for a more in-depth performance status evaluation of an older person with cancer was identified over 20 years ago, completion of a comprehensive geriatric assessment (CGA) is time-consuming and not frequently performed as part of the standard assessment of older cancer patients. Evidence suggests that incorporating such an evaluation could be useful for potentially determining the patient’s chemotherapy tolerability or treatment completion, toxicity, and survival, as age alone has been shown to poorly predict treatment failure, and performance status assessments commonly used in oncology practice may lack predictability. This review describes the increasing role of the CGA and geriatric assessment screening tools as well as their pertinent domains across various settings in the evaluation of the older adult with cancer who is considering cancer treatment.
Introduction
The majority of cancer diagnoses and morbidity occurs in patients age 65 and older.[1] Elderly patients remain under-represented in cancer clinical trials and undertreated clinically for cancer, despite evidence that they experience similar chemotherapy efficacy to younger adults.[2–5] This may be related to the perception of increased risk for toxicity that can occur in some older adults. While there may be concern that elderly patients experience increased toxicities with treatment, this is likely not the case for all patients. The aging population is growing, and designing appropriate clinical trials that are more inclusive, in addition to recommending trials to elderly patients who might be eligible, continues to be an emerging need.
In the context of cancer treatment, older adults have several disadvantages when compared to their younger cohorts. They are more likely to have baseline comorbidities, they take more medications, and they may not tolerate chemotherapy as well as younger patients. These factors can complicate their treatment and render cancer therapy decisions in older patients, particularly challenging.[6]
Presently, most oncologists rely on global assessment measures such as Karnofsky Performance Status (KPS) or the Eastern Cooperative Oncology Group Performance Status (ECOG PS) tool to determine a patient’s performance status, and subsequently, their eligibility for chemotherapy or clinical trial participation. The thought is that individuals who are too frail to benefit would be affected by undesirable side effects and should not be enrolled. However, these tools may not be sufficient when assessing the older adult’s potential to undergo chemotherapy.
The comprehensive geriatric assessment (CGA) is an evaluation method used by geriatricians to describe the multidisciplinary assessment of an older patient. The CGA can be applied to the evaluation of an older patient considering chemotherapy or can also be potentially applied towards assessing an elderly patient’s eligibility for a clinical trial, given that it is more thorough and tailored to the needs and problems of older patients as compared to KPS, for instance. There is evidence that using such an assessment as a tool can more accurately predict outcome compared to ECOG PS or KPS.[7,8] In this review, CGA and geriatric assessment (GA) will be used synonymously, however, GA has also been used to describe abbreviated versions of a CGA with select elements or domains of focus differing among investigators, as will be described.
Specifically, the CGA involves the assessment of an individual’s functional status; comorbidities, including fall risk; cognition; psychosocial state; social support; nutritional status; and it also includes a medication review. Functional status is typically evaluated by appraising somebody’s independence in Activities of Daily Living (ADLs) and Instrumental ADLs (IADL). Comorbidities and fall risk are integrated into the physical examination of the geriatric patient, with gait speed and balance evaluations often included in the fall-risk assessment. The Mini Mental State Examination (MMSE) and the Montreal Cognitive Assessment (MOCA) are widely-used tools that screen for cognitive impairment and provide a metric on cognitive function. Depression can be screened by a short questionnaire known as the Patient Health Questionnaire (PHQ2) or a geriatric depression scale (GDS). Social Support can be briefly assessed in the social history inquiry. Besides the patient history, screening for malnutrition and weight loss can be performed by an 18-item Mini-Nutritional Assessment (MNA) tool [9] or a simplified nutrition assessment questionnaire. Furthermore, a CGA includes a review of the patient’s medications at each visit, as polypharmacy can be a problem among the elderly.
Functional status assessments such as KPS can miss elderly patients with cancer who might be rated as functionally normal by that measure but have deficits identified on a CGA, and such deficits could affect treatment tolerance and patient outcomes.[8] Geriatric assessments, in a prospective study, were found to predict overall survival (OS) better than KPS, in elderly cancer patients.[7] Others present evidence on how the CGA can detect issues not reflected in ECOG assessments and how impairments in geriatric domains have predictive value for mortality and chemotherapy completion in older patients with cancer.[10]
The incorporation of a CGA in the evaluation and care of the senior adult with cancer acknowledges and may address some of the common, age-associated conditions occurring in the elderly. Addressing geriatric syndromes or impairments identified in a CGA could have a positive impact on outcomes such as chemotherapy completion, morbidity or mortality, as well as on the frequency of emergency department visits and hospitalization rates among elderly cancer patients.[11] This review will describe the increasing role of the use of a CGA and its pertinent variables in the evaluation of the older adult with cancer.
Comprehensive Geriatric Assessment and Select Geriatric Assessment Tools in the Oncology Practice
Geriatric assessments have now been recommended in the evaluation of an older adult considering cancer therapy,[12,13] and the evidence is mounting with respect to the utility of the CGA in oncology practice.[14–16] Unfortunately, the incorporation of the CGA in the oncology practice remains infrequent.[17]
While the need for a more in-depth evaluation of an older person with cancer was identified over 20 years ago,[18,19] completion of a CGA is time-consuming and may not be feasible in the standard care of patients, resulting in its infrequent implementation. Initially, the use of a CGA in the care of the elderly cancer patient originated from extrapolating its ability to predict morbidity and mortality in the general geriatric population.[20] Older adults often suffer from common health conditions that have multifactorial causes, referred to as geriatric syndromes. Cognitive impairment, delirium, incontinence, malnutrition, falls, gait disorders, pressure ulcers, sleep disorders, sensory deficits, fatigue, and dizziness frequently ail the older adult. Geriatric syndromes can be identified by a CGA.[21] This evaluation can identify impairments across several domains that may contribute to the vulnerability and adverse outcomes of older individuals. [20,22]
Incorporating such an evaluation into the oncology practice could be useful in determining who might tolerate chemotherapy, who would be susceptible to toxicity, or what factors, if addressed, could increase the likelihood of completing treatment, as age itself has been shown to poorly predict treatment failure.[23,24] Because a CGA is a multi-component evaluation, it would not appear to be practical in a busy oncology practice. An abbreviation or modification of a CGA is an approach that can be adopted to make the assessment feasible in routine cancer care. Ingram et al. and Hurria et al. were among the first to describe the feasibility of incorporating a GA in the evaluation of a cancer patient.[25,26] In their study, Hurria and others suggest that a GA can reasonably be incorporated into the busy oncology practice, with the majority of the assessment being self-administered. A mean time of 27 minutes (range: 8-45 minutes) to completion of the assessment was reported by that group.[26] Others have also determined that performing a brief GA in the community oncology setting is a feasible task.[27] Specific attributes or elements that comprise the CGA may confer greater utility than others, and select, more relevant domains can also be incorporated into screening tools that would be briefer than a CGA. Consequently, these tools could be quickly administered in an outpatient setting.[15] Similar tools have also been suggested to be feasible in the inpatient setting,[28] as well as in a variety of settings.[29] There are specific domains within a GA that have been shown to be predictive of chemotherapy toxicity when examined by Hurria [16,30] and others[31] and ultimately, resulted in the development of toxicity predictor tools such as the Cancer and Aging Research Group (CARG) toxicity tool[16] and the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score.[31] In particular, the CARG chemotherapy toxicity score is a validated tool that predicts the likelihood of chemotherapy toxicity and incorporates cancer and treatment-specific variables in addition to domains from the CGA, such as history of falls and difficulties with medication management.[16] Whereas the CRASH score includes several CGA risk factors such as IADL dependence and impaired cognition. In addition, these tools have also been shown to be superior to assessments commonly used in oncology practice that determine eligibility for chemotherapy (e.g. ECOG, KPS).[30]
A modified CGA tool demonstrated superiority as compared with the oncologist’s clinical judgment in identifying frailty. Kirkhus et al. revealed that frailty assessed by a modified GA --where patients were defined as frail if they met one of the following criteria: dependencies in ADLs, significant comorbidity, polypharmacy, physical function, or having one or more geriatric syndrome -- was independently prognostic for survival, compared with oncologists’ subjective classification. Agreement between the modified CGA and the oncologist’s assessment was reported as fair, using kappa statistics (kappa value 0.30 [95% CI, 0.19; 0.41]), and only the modified tool’s determination of frailty was independently prognostic for survival.[32] An abridged CGA, in a prospective study, was also found to be a better predictor of OS as compared to KPS, and in fact, the assessment tool was the only one that resulted being predictive of mortality of elderly patients.[7] Further, KPS assessments can potentially miss older cancer patients who might be rated as functionally normal by that measure but have deficits identified by a GA; these deficits could affect treatment tolerance and patient outcomes.[8] This is possibly related to the fact that KPS does not include a cognition assessment that may impact treatment adherence nor a nutritional assessment or social support inquiry which may influence tolerance and therapy completion.
Another notable aspect is the suggestion that older patients can be assigned lower performance status scores compared to their younger cohorts, even when measured physical activity may not differ between the two groups.[33,34] This highlights the potential of adopting a CGA to evaluate an older cancer patient and also suggests its superiority to commonly employed assessments of performance status (e.g. KPS).
Subsequent tools have emerged that involve an abbreviated CGA to assess geriatric cancer patients. Martinez-Tapia et al. evaluated the G8 and modified-G8 screening tools (tools that elicit items on nutrition, mobility, falls, polypharmacy, cognition) in a European study and revealed that abnormal scores were strong and consistent predictors of OS, regardless of metastatic status or tumor site.[33] The G8 score tool was validated in the ONCODAGE French prospective study that included adults ≥ 70 years .with several solid malignancies and a minority (7.8%) of lymphoma patients.[35]
Diversity of Settings and Malignancies Using CGA Tools or Its Variables in Older Patients with Cancer
Several additional studies have illustrated the value of using a variation of the CGA or elements within a CGA in the geriatric oncology setting and in various cancer types and stages. In one of the landmark studies where the majority of patients had solid malignancies (81%), the abbreviated assessment was largely self-administered.[26] While subsequent earlier studies of CGAs in the context of cancer were initially performed in predominantly-solid malignancies, applications in hematologic malignancies have been progressively increasing over time and have demonstrated the utility of these tools,[11,24,26,28,36-51] as shown in the Table.
Solid Malignancies
Among the individual variables within a CGA that have resulted in abridged tools, slow gait speed has been shown to be an independent predictor of early death in older cancer patients with predominantly (98%) solid malignancies.[52] In patients ≥ 65 years (median age of 73), who had primarily lung, breast or colorectal cancer, a brief GA prior to chemotherapy was associated with completion of chemotherapy by 67.6% of the participants.[43] Visual and hearing impairments are additional variables that were found to have prognostic value among older oncology patients, [7] as was cognitive impairment, which was found to predict survival at the initiation of treatment (hazard ratio [HR] = 6.13; 95% confidence interval [CI] = 2.07-18.09; P = .001).[44] Paillaud et al. in a prospective study found a link between metastasis and malnutrition evaluated by an MNA in those with non-digestive malignancies (adjusted odds ratio [ORa] = 25.25; 95%CI, 5.97-106.8).[45]
GI
A randomized study of metastatic colorectal carcinoma elderly patients demonstrated the MMSE (OR, 3.84) and impaired instrumental activities of daily living (IADLs (OR, 4.67) to be predictive of severe toxicity, with the MMSE (OR, 4.56) and Geriatric Depression Scale (OR, 5.52) being predictive of unexpected hospitalizations, suggesting cognitive function, independence impairment and depression to be important factors that should be considered when choosing a chemotherapy regimen in older adults.[11] In a separate study, a mini CGA performed by gastroenterologists was shown to be useful in adapting the anticancer treatments of elderly patients with digestive cancers.[46]
Lung
Schulkes and his group examined evidence from 18 studies and in their review, highlight how the CGA can detect issues not reflected in ECOG assessments and how impairments in geriatric domains such as physical capacity, nutritional status, cognition and IADL impairment have predictive value for mortality and chemotherapy completion in lung cancer patients.[10]
Breast
A CGA was also useful in predicting tolerance of treatment, mortality[47] and 3-year survival in geriatric patients with breast cancer.[53] Interestingly, Okonji and others evaluated CGAs in 326 women ≥ 70 years with breast cancer and found under-treatment in this group. Nearly 50% of fit women with high risk disease did not receive adjuvant chemotherapy.[54] This may allude to a hesitancy of oncologists to treat advanced-age patients, partly due to current, imperfect methods that are commonly used to assess these patients prior to chemotherapy initiation (e.g. KPS, ECOG). In the metastatic breast cancer setting, van de Water et al. maintain that a geriatric oncology approach might improve survival in elderly patients because 3-year mortality was 13% lower than for those receiving a standard approach.[55]
Prostate
Among the patients who are deemed candidates for treatment, a CGA may facilitate the identification of those who are at risk for therapy discontinuation. When elderly patients with prostate cancer were assessed for frailty by CGAs, a statistically-significant relationship between frailty assessed by CGA and early docetaxel discontinuation was found.[56].
Ovarian Cancer
A prospective study of older (median age of 76 years) patients with advanced ovarian cancer in which CGAs were used, showed domains such as depression (P = .003) and polypharmacy (P = .043) to be independent predictors of toxicity and OS.[48]
Hematologic Malignancies
Studies incorporating GAs in the evaluation of patients with hematologic malignancies have followed those performed in patients with solid malignancies (Table). A recent analysis maintains that pretreatment CGAs accurately predict survival and treatment related toxicities in geriatric patients with diffuse large B cell lymphoma (DLBCL) who received anthracycline-based therapy, and treating them with anthracycline-containing regimens was associated with a three-year OS rate of 63% vs 44% for anthracycline-free regimens.[57] Ribi et al. also evaluated a “cancer specific” GA and quality of life in older patients with aggressive B cell lymphomas receiving rituximab-bendamustine-lenalidomide (R-BL) and determined that pre-treatment impaired functional status was an important factor of clinical outcomes, as 53% of patients who died had pre-treatment impaired functional status (vs. 0%, P = .003).[40] Additionally, a retrospective analysis suggested that certain factors affected survival in non-Hodgkin lymphoma (NHL). Comorbidity scores ≥ 6, doxorubicin exclusion, and cognitive impairment were strongly associated with survival in NHL[49] It is of interest that besides having predictive value, application of the CGA to the hematologic malignancy setting could be used to adjust a treatment regimen, possibly impacting outcomes. This was exemplified by Spina et al., who suggest that the use of a CGA can be used to adjust chemoimmunotherapy, with potentially better cure rates in fit and unfit patients. In their study of 100 DLBCL patients, 81% of patients had a complete response and mild toxicity was seen in only 17%.[50]
Individual elements within a CGA have been studied in hematologic malignancies and may also have predictive potential. The timed-up-and-go test (a measure of gait speed) was found to be strongly associated with poor survival in a German study of 75 patients with chronic lymphocytic leukemia (CLL). Median OS was found to be 53.8 months in those with speeds less than or equal to 10 seconds vs 18.2 months for those with twice the gait speed.[51] Hand grip strength is yet another variable that has been correlated with frailty in geriatric hematology patients. Velghe et al. proposed using grip strength as a screening tool after having revealed it to be associated with a concurrent abnormal CGA (P = .058 and .009 for women and men, respectively).[41] Park and others determined that an MNA comprised of a short form assessment was predictive of tolerability to multi-agent chemotherapy involving CHOP (cyclophosphamide, doxorubicin, vincristine, prednisone) or “CHOP-like” regimens in elderly patients with aggressive NHL;[42] whereas Aaldriks et al. showed that both an inferior MNA and a mini cognitive screen (MMSE) were predictive of chemotherapy discontinuation (P = .001 and 0.04, respectively) with an inferior MNA presenting an increased mortality risk (HR = 2.19 ) after initiation of chemotherapy in patients with predominantly hematologic malignancies.[37]
Upon conducting a search in PubMed and Medline in November 2017, using the medical subject headings (MeSH) terms geriatric assessment AND oncology OR cancer, with limits of the search restricted to the human species, collectively, the majority of the studies suggest utility of a CGA in the assessment of an elderly cancer patient. There were, however, a few instances where a CGA did not have benefit, in terms of predictive value. Osborne et al. found that a CGA did not predict acute radiotherapy toxicity in men ≥ 70 years with localized prostate cancer.[58] It is possible that because the mechanisms for radiotoxicity are different from those involving chemotherapy or targeted therapy, a CGA may not identify patients at risk of radiotoxicity. This point highlights how the specificity of a particular treatment could affect results, and it illustrates the consideration that a CGA may have a role in certain regimens but less relevance in others. Guion-Dusserre and others, for example, did not find geriatric parameters within a CGA to be linked to OS in older patients with pancreatic or colorectal cancer who were treated with FOLFIRINOX (leucovorin, fluorouracil, irinotecan, oxaliplatin).[59] In one study of 494 patients with advanced non-small cell lung cancer, results suggested that treatment allocation based on a CGA did not improve treatment failure free survival or OS, but did slightly reduce treatment toxicity.[60]
Although diverse and in multiple cancer types, these studies have not typically involved the gold-standard study design: the randomized clinical trial. The first multicenter, randomized clinical trial (NCT02025062) using a CGA in elderly patients with head and neck cancer is currently in the recruitment phase.[61] More importantly, whether managing the deficits detected on screening results in a meaningful impact, remains inconclusive, as illustrated by a French study in which dietary counseling was provided to at-risk patients who had been identified on a nutritional screen, but such counseling had no significant effect on mortality, toxicity or chemotherapy outcomes.[63] (this reference is a falls-risk reference instead of the Bourdel et al. study, listed as #62 in this version)
Intervention after Identifying Abnormal Screenings on CGA or CGA Tools
Although CGA screens followed by management interventions have not been evaluated at length in randomized studies in geriatric oncology patients, several studies in the non-cancer setting report a benefit of incorporating CGA-prompted management and may also represent benefit in the oncology setting.[22,63–65] Geriatric assessment management interventions are employed by geriatricians to support or reverse any identified impairments. Similarly, impairments detected in the evaluation of an older cancer patient who is about to start chemotherapy can be addressed. Magnuson et al. recently conducted a randomized pilot study comparing GA with management interventions versus usual care in patients with stage III/IV solid tumor malignances, and in that study, it was discovered that the incidence of grade 3-5 chemotherapy toxicity did not differ between the two groups. Prevalence of dose reduction, dose delays, hospitalization, and early treatment discontinuation also was not different between groups; however, the recommendations made to the primary oncologist by geriatricians had a low implementation rate.[66] It is possible that if execution of recommendations had been greater or if barriers to implementations had been identified, intervention could have led to improved outcomes. Notable is the fact that the sample size of that pilot study was modest (N = 71) and thus, differences may have not been detected with that sample size or in a pilot study design. Further, the two study arms were not balanced, given that the intervention arm had higher rates of IADL impairment and greater frequency of high-risk CARG toxicity scores, possibly minimizing the benefit of intervention. That study proved to be a feasible one, however, and recommendations for referrals that were more easily attainable (e.g. social work consults, nutrition consults) were implemented at a higher frequency compared to more “geriatric-specific” recommendations.
In a different study of CGA evaluation with intervention for reducing toxicity in older patients with advanced cancer, Kalsi et al. observed benefit from intervention with respect to chemotherapy tolerance, albeit in a non-randomized trial design. The authors revealed that the geriatrician-led CGA interventions were associated with improved chemotherapy tolerance and that patients were more likely to complete treatment (odds ratio, 4.14) with lower toxicity rates observed (43.8%) vs the non-intervention group (52.9%).[67] Although intuitive, whether intervening after detecting deficits identified in a CGA or CGA-abbreviated tools could impact outcomes in the oncology setting, remains unclear. No significant effect on OS was found when intervention was performed in the non-cancer population in a trial of 1388 patients, although intervention appeared to reduce functional decline and improve mental health without added costs.[68] As discussed, in the context of cancer, a study in which dietary counseling of elderly patients with cancer was offered had no effect on mortality or chemotherapy outcomes (e.g. progression, remission),[62] pointing to the need to further evaluate the effect of CGA-prompted interventions in oncology settings.
Future Research
The elderly remain under-represented in cancer clinical trials. The need for inclusion of older patients in clinical studies and determining their treatment eligibility is a recurrent theme that is being highlighted more and more frequently. Many, such as Hurria, Extermann, Balducci, Power, Lichtman and others, emphasize the urgent need to include older patients in clinical trials and to employ the CGA in the oncology setting to better understand its use in identifying patients who would likely derive benefits.[1,15,16,20,69] Ideally, trials that involve management of deficits identified on screening could help answer the question as to whether interventions have a significant impact on cancer outcomes. As mentioned, a randomized trial involving patients with head and neck cancer with intervention strategies is in progress (NCT02025062). Similarly, a trial that evaluates the feasibility of a midlevel practitioner to develop and implement GA-management interventions is also under way (NCT02517034). The current evidence predominantly supports the benefit of incorporating CGAs or abbreviated tools in the evaluation of the elderly cancer patient; this task appears to be feasible in the routine oncology setting.
It also remains to be determined more definitively whether there are cancer types or specific treatment regimens in which CGAs would confer the largest benefit. Bamias et al. suggest that a CGA might be useful to select patients with advanced urothelial carcinoma unfit for cisplatin who may be likely to benefit from first-line gemcitabine/carboplatin combinations [70], for example. More importantly, it remains to be determined whether identifying deficits on a CGA screen is consequential and intervening and addressing such deficits would alter outcomes of older cancer patients.[50,51] A CGA is comprised of multiple elements, across several domains and identifying the individual elements within a CGA that could have the greatest predictive value in the right setting or whether intervening on that single element is of benefit could prove to be challenging.
Conclusions
The CGA is being considered with greater frequency in the geriatric oncology setting since it was first proposed for this scenario. The CGA is now often implemented as a brief screening tool or cancer-specific GA tool whose limited domains can quickly be employed to assess the older cancer patient who is about to undergo a standard or experimental treatment regimen. Further research including randomized trials and interventional trials are needed to better identify the more cancer-relevant domains within a CGA and to clarify the cancer types and specific chemotherapy regimens in which oncology-themed CGA tools would confer the greatest utility.
Acknowledgements: We thank Dr. Tapasya Raavi for his assistance with the preparation of this manuscript and Mr. Thomas Bartholomew for his edits as well as Drs. Maria Ribeiro, Anna Mirk, Javier Pinilla and Lubomir Sokol for their support and guidance.
Financial Disclosure: This material is the result of work supported by the Advanced Fellowship Program with resources and the use of facilities at the Atlanta VA Medical Center. The authors do not have any other financial disclosures.
FIVE KEY REFERENCES
7. Ghosn M, Ibrahim T, El Rassy E, et al. Abridged geriatric assessment is a better predictor of overall survival than the Karnofsky Performance Scale and Physical Performance Test in elderly patients with cancer. J Geriatr Oncol. 2017;8:128-32.
8. Jolly TA, Deal AM, Nyrop KA, et al. Geriatric assessment-identified deficits in older cancer patients with normal performance status. Oncologist. 2015;20:379-85.
11. Aparicio T, Jouve JL, Teillet L, et al. Geriatric factors predict chemotherapy feasibility: ancillary results of FFCD 2001-02 phase III study in first-line chemotherapy for metastatic colorectal cancer in elderly patients. J Clin Oncol. 2013;31:1464-70.
33. Martinez-Tapia C, Paillaud E, Liuu E, et al. Prognostic value of the G8 and modified-G8 screening tools for multidimensional health problems in older patients with cancer. Eur J Cancer. 2017;83:211-9.
66. Magnuson A, Lemelman T, Pandya C, et al. Geriatric assessment with management intervention in older adults with cancer: a randomized pilot study. Support Care Cancer. 2018;26:605-13.
PERSPECTIVE

Geriatric Assessment: How can we increase implementation?
Erika Ramsdale, MD
A geriatric assessment (GA) is now recommended by for all older adults receiving chemotherapy, in a clinical practice guideline released by the American Society of Clinical Oncology (ASCO).1 As the accompanying review article discusses, GA can detect vulnerabilities not identified by a routine oncologic assessment, and it outperforms common tools such as the Eastern Cooperative Oncology Group (ECOG) and Karnofsky performance status in predicting outcomes including survival and chemotherapy toxicity.2-4> The Comprehensive Geriatric Assessment (CGA) is not always needed; a shorter GA with selected elements can provide valuable information for many older patients, as outlined in the ASCO guideline.1 Despite strong evidence supporting implementation, less than 25% of community oncologists in the United States report using GA for their older patients.5
In my interviews with oncologists across the country about implementation of GA, time and resource limitations were frequently cited as barriers. However, surprisingly, oncologists more frequently cited a lack of buy-in as a barrier: they either did not believe that GA could add information to their assessment of a patient’s functioning, or they felt unsure about how to interpret and act on GA information.6 Given the dearth of geriatricians nationwide,7 it is important that we investigate how best to disseminate and implement GA and GA-driven interventions within oncology clinics.
One potential implementation could emerge from information technologies such as the electronic medical record (EMR). Most GA elements are patient-reported, and older adults are growing increasingly comfortable with digital technologies.8 We are investigating the use of EMR-integrated GA in our oncology clinics. The patients can complete the instruments in their own homes, via a web-based portal, or in the waiting room on a tablet computer, with data fed to the EMR. The EMR could further be leveraged to score instruments, view longitudinal changes, provide individualized recommendations, and/or link to automated order sets. If implemented thoughtfully, an EMR-integrated GA could offload busy oncologists and provide information support and data analysis. This, in turn, will support treatment decision-making and beneficial outcomes for older adults with cancer.
FIVE KEY REFERENCES
1. Mohile SG, Dale W, Somerfield MR, Hurria A. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology Summary. J Oncol Pract 2018; 14(7): 442-6.
2. Ghosn M, Ibrahim T, El Rassy E, Nassani N, Ghanem S, Assi T. Abridged geriatric assessment is a better predictor of overall survival than the Karnofsky Performance Scale and Physical Performance Test in elderly patients with cancer. J Geriatr Oncol 2017; 8(2): 128-32.
5. Mohile SG, Magnuson A, Pandya C, et al. Community Oncologists’ Decision-Making for Treatment of Older Patients With Cancer. J Natl Compr Canc Netw 2018; 16(3): 301-9.
6. Ramsdale E, Arastu A, Narlock G, et al. “People are shocked and then they start using it”: Oncology Providers’ Perceived Barriers to Implementation of the Geriatric Assessment. Journal of Geriatric Oncology 2018; 9(6): S123-S4.
7. American Geriatrics Society. State of the Geriatrician Workforce. Accessed August 29, 2019 at https://www.americangeriatrics.org/geriatrics-profession/about-geriatrics/geriatrics-workforce-numbers.
Dr. Ramsdale is a Medical Oncologist and Assistant Professor of Medicine, University of Rochester, James P. Wilmot Cancer Institute, Rochester, New York.
References:
1. Balducci L, Ershler WB. Cancer and ageing: a nexus at several levels. Nature Rev Cancer. 2005;5:655-62.
2. Sundararajan V, Mitra N, Jacobson JS, et al. Survival associated with 5-fluorouracil-based adjuvant chemotherapy among elderly patients with node-positive colon cancer. Ann Intern Med. 2002;136:349-57.
3. Jessup JM, Stewart A, Greene FL, Minsky BD. Adjuvant chemotherapy for stage III colon cancer: implications of race/ethnicity, age, and differentiation. JAMA. 2005;294:2703-11.
4. Bouvier AM, Jooste V, Bonnetain F, et al. Adjuvant treatments do not alter the quality of life in elderly patients with colorectal cancer: a population-based study. Cancer. 2008;113:879-86.
5. Haller DG, Catalano PJ, Macdonald JS, et al. Phase III study of fluorouracil, leucovorin, and levamisole in high-risk stage II and III colon cancer: final report of Intergroup 0089. J Clin Oncol. 2005;23:8671-8.
6. Li D, de Glas NA, Hurria A. Cancer and aging: general principles, biology, and geriatric assessment. Clin Geriatr Med. 2016;32:1-15.
7. Ghosn M, Ibrahim T, El Rassy E, et al. Abridged geriatric assessment is a better predictor of overall survival than the Karnofsky Performance Scale and Physical Performance Test in elderly patients with cancer. J Geriatr Oncol. 2017;8:128-32.
8. Jolly TA, Deal AM, Nyrop KA, et al. Geriatric assessment-identified deficits in older cancer patients with normal performance status. Oncologist. 2015;20:379-85.
9. Nestlé Nutrition Institute. MNA® mini nutritional assessment. Available at: http://www.mna-elderly.com. Accessed June 25, 2018.
10. Schulkes KJ, Hamaker ME, van den Bos F, van Elden LJ. Relevance of a geriatric assessment for elderly patients with lung cancer-a systematic review. Clin Lung Cancer. 2016;17:341-349.e3.
11. Aparicio T, Jouve JL, Teillet L, et al. Geriatric factors predict chemotherapy feasibility: ancillary results of FFCD 2001-02 phase III study in first-line chemotherapy for metastatic colorectal cancer in elderly patients. J Clin Oncol. 2013;31:1464-70.
12. Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55:241-52.
13. Hurria A, Browner IS, Cohen HJ, et al. Senior adult oncology. J Natl Compr Canc Netw. 2012;10:162-209.
14. Wildiers H, Heeren P, Puts M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014;32:2595-603.
15. Hurria A, Lichtman SM, Gardes J, et al. Identifying vulnerable older adults with cancer: integrating geriatric assessment into oncology practice. J Am Geriatr Soc. 2007;55:1604-8.
16. Hurria A, Cirrincione CT, Muss HB, et al. Implementing a geriatric assessment in cooperative group clinical cancer trials: CALGB 360401. J Clin Oncol. 2011;29:1290-6.
17. Lakhanpal R, Yoong J, Joshi S, et al. Geriatric assessment of older patients with cancer in Australia--a multicentre audit. J Geriatr Oncol. 2015;6:185-93.
18. Reuben DB. Geriatric assessment in oncology. Cancer. 1997;80:1311-6.
19. Roche RJ, Forman WB, Rhyne RL. Formal geriatric assessment: an imperative for the older person with cancer. Cancer Pract. 1997;5:81-6.
20. Extermann M, Hurria A. Comprehensive geriatric assessment for older patients with cancer. J Clin Oncol. 2007;25:1824-31.
21. Ward KT, Reuben DB. Comprehensive geriatric assessment. - UpToDate. Available from: https://www.uptodate.com/contents/comprehensive-geriatric-assessment?search=comprehensive%20geriatric%20assessment&source=search_result&selectedTitle=1~66&usage_type=default&display_rank=1. Accessed June 26, 2018.
22. Magnuson A, Allore H, Cohen HJ, et al. Geriatric assessment with management in cancer care: current evidence and potential mechanisms for future research. J Geriatr Oncol. 2016;7:242-8.
23. Klepin H, Mohile S, Hurria A. Geriatric assessment in older patients with breast cancer. J Nat Compr Canc Netw. 2009;7:226-36.
24. Marinello R, Marenco D, Roglia D, et al. Predictors of treatment failures during chemotherapy: a prospective study on 110 older cancer patients. Arch Gerontol Geriatr. 2009;48:222-6.
25. Ingram SS, Seo PH, Martell RE, et al. Comprehensive assessment of the elderly cancer patient: the feasibility of self-report methodology. J Clin Oncol. 2002;20:770-5.
26. Hurria A, Gupta S, Zauderer M, et al. Developing a cancer-specific geriatric assessment: a feasibility study. Cancer. 2005;104:1998-2005.
27. Williams GR, Deal AM, Jolly TA, et al. Feasibility of geriatric assessment in community oncology clinics. J Geriatr Oncol. 2014;5:245-51.
28. Klepin HD, Geiger AM, Tooze JA, et al. The feasibility of inpatient geriatric assessment for older adults receiving induction chemotherapy for acute myelogenous leukemia. J Am Geriatr Soc. 2011;59:1837-46.
29. Liu JJ, Extermann M. Comprehensive geriatric assessment and its clinical impact in oncology. Clin Geriatr Med. 2012;28:19-31.
30. Hurria A, Mohile S, Gajra A, et al. Validation of a prediction tool for chemotherapy toxicity in older adults with cancer. J Clin Oncol. 2016;34:2366-71.
31. Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer. 2012;118:3377-86.
32. Kirkhus L, Saltyte Benth J, Rostoft S, et al. Geriatric assessment is superior to oncologists’ clinical judgement in identifying frailty. Br J Cancer. 2017;117:470-7.
33. Martinez-Tapia C, Paillaud E, Liuu E, et al. Prognostic value of the G8 and modified-G8 screening tools for multidimensional health problems in older patients with cancer. Eur J Cancer. 2017;83:211-9.
34. Broderick JM, Hussey J, Kennedy MJ, O’Donnell DM. Patients over 65 years are assigned lower ECOG PS scores than younger patients, although objectively measured physical activity is no different. J Geriatr Oncol. 2014;5:49-56.
35. Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PLoS One. 2014;9:e115060.
36. Kim YJ, Kim JH, Park MS, et al. Comprehensive geriatric assessment in Korean elderly cancer patients receiving chemotherapy. J Cancer Res Clin Oncol. 2011;137:839-47.
37. Aaldriks AA, Maartense E, le Cessie S, et al. Predictive value of geriatric assessment for patients older than 70 years, treated with chemotherapy. Crit Rev Oncol Hemat. 2011;79:205-12.
38. Clough-Gorr KM, Thwin SS, Stuck AE, Silliman RA. Examining five- and ten-year survival in older women with breast cancer using cancer-specific geriatric assessment. Eur J Cancer. 2012;48:805-12.
39. Caillet P, Canoui-Poitrine F, Vouriot J, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J Clin Oncol. 2011;29:3636-42.
40. Ribi K, Rondeau S, Hitz F, et al. Cancer-specific geriatric assessment and quality of life: important factors in caring for older patients with aggressive B-cell lymphoma. Support Care Cancer. 2017;25:2833-42.
41. Velghe A, De Buyser S, Noens L, Demuynck R, Petrovic M. Hand grip strength as a screening tool for frailty in older patients with haematological malignancies. Acta Clin Belg. 2016;71:227-30.
42. Park S, Hong J, Hwang I, et al. Comprehensive geriatric assessment in elderly patients with newly diagnosed aggressive non-Hodgkin lymphoma treated with multi-agent chemotherapy. J Geriatr Oncol. 2015;6:470-8.
43. Wildes TM, Ruwe AP, Fournier C, et al. Geriatric assessment is associated with completion of chemotherapy, toxicity, and survival in older adults with cancer. J Geriatr Oncol. 2013;4:227-34.
44. Libert Y, Dubruille S, Borghgraef C, et al. Vulnerabilities in older patients when cancer treatment is initiated: Does a cognitive impairment impact the two-year survival? PLoS One. 2016;11:e0159734.
45. Paillaud E, Liuu E, Laurent M, et al. Geriatric syndromes increased the nutritional risk in elderly cancer patients independently from tumour site and metastatic status. The ELCAPA-05 cohort study. Clin Nutr. 2014;33:330-5.
46. Aparicio T, Girard L, Bouarioua N, et al. A mini geriatric assessment helps treatment decision in elderly patients with digestive cancer. A pilot study. Crit Rev Oncol Hematol. 2011;77:63-9.
47. Clough-Gorr KM, Stuck AE, Thwin SS, Silliman RA. Older breast cancer survivors: geriatric assessment domains are associated with poor tolerance of treatment adverse effects and predict mortality over 7 years of follow-up. J Clin Oncol. 2010;28:380-6.
48. Freyer G, Geay JF, Touzet S, et al. Comprehensive geriatric assessment predicts tolerance to chemotherapy and survival in elderly patients with advanced ovarian carcinoma: a GINECO study. Ann Oncol. 2005;16:1795-800.
49. Naito Y, Sasaki H, Takamatsu Y, Kiyomi F, Tamura K. Retrospective analysis of treatment outcomes and geriatric assessment in elderly malignant lymphoma patients. J Clin Exp Hematop. 2016;56:43-9.
50. Spina M, Balzarotti M, Uziel L, et al. Modulated chemotherapy according to modified comprehensive geriatric assessment in 100 consecutive elderly patients with diffuse large B-cell lymphoma. Oncologist. 2012;17:838-46.
51. Goede V, Bahlo J, Chataline V, et al. Evaluation of geriatric assessment in patients with chronic lymphocytic leukemia: results of the CLL9 trial of the German CLL study group. Leuk Lymphoma. 2016;57:789-96.
52. Pamoukdjian F, Levy V, Sebbane G, et al. Slow gait speed is an independent predictor of early death in older cancer outpatients: results from a prospective cohort study. J Nutr Health Aging. 2017;21:202-6.
53. Stotter A, Reed MW, Gray LJ, Moore N, Robinson TG. Comprehensive Geriatric Assessment and predicted 3-year survival in treatment planning for frail patients with early breast cancer. Br J Surg. 2015;102:525-33; discussion 533.
54. Okonji DO, Sinha R, Phillips I, Fatz D, Ring A. Comprehensive geriatric assessment in 326 older women with early breast cancer. Br J Cancer. 2017;117:925-31.
55. van de Water W, Bastiaannet E, Egan KM, et al. Management of primary metastatic breast cancer in elderly patients--an international comparison of oncogeriatric versus standard care. J Geriatr Oncol. 2014;5:252-9.
56. Della Pepa C, Cavaliere C, Rossetti S, et al. Predictive Comprehensive Geriatric Assessment in elderly prostate cancer patients: the prospective observational scoop trial results. Anticancer Drugs. 2017;28:104-9.
57. Lin RJ, Behera M, Diefenbach CS, Flowers CR. Role of anthracycline and comprehensive geriatric assessment for elderly patients with diffuse large B-cell lymphoma. Blood. 2017;130:2180-5.
58. Osborne GEC, Appleyard SA, Gilbert DC, et al. Comprehensive geriatric assessment in men aged 70 years or older with localised prostate cancer undergoing radical radiotherapy. Clin Oncol. 2017;29:609-16.
59. Guion-Dusserre JF, Bertaut A, Ghiringhelli F, et al. Folfirinox in elderly patients with pancreatic or colorectal cancer-tolerance and efficacy. World J Gastroenterol. 2016;22:9378-86.
60. Corre R, Greillier L, Le Caer H, et al. Use of a comprehensive geriatric assessment for the management of elderly patients with advanced non-small-cell lung cancer: The phase III randomized ESOGIA-GFPC-GECP 08-02 study. J Clin Oncol. 2016;34:1476-83.
61. Brugel L, Laurent M, Caillet P, et al. Impact of comprehensive geriatric assessment on survival, function, and nutritional status in elderly patients with head and neck cancer: protocol for a multicentre randomised controlled trial (EGeSOR). BMC Cancer. 2014;14:427.
62. Bourdel-Marchasson I, Blanc-Bisson C, Doussau A, et al. Nutritional advice in older patients at risk of malnutrition during treatment for chemotherapy: a two-year randomized controlled trial. PLoS One. 2014;9:e108687.
63. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012 Sep 12;(9):CD007146.
64. Nykänen I, Rissanen TH, Sulkava R, Hartikainen S. Effects of individual dietary counseling as part of a comprehensive geriatric assessment (CGA) on nutritional status: a population-based intervention study. J Nutr Health Aging. 2014;18:54-8.
65. Keeler EB, Robalino DA, Frank JC, et al. Cost-effectiveness of outpatient geriatric assessment with an intervention to increase adherence. Med Care. 1999;37:1199-206.
66. Magnuson A, Lemelman T, Pandya C, et al. Geriatric assessment with management intervention in older adults with cancer: a randomized pilot study. Support Care Cancer. 2018;26:605-13.
67. Kalsi T, Babic-Illman G, Ross PJ, et al. The impact of comprehensive geriatric assessment interventions on tolerance to chemotherapy in older people. Br J Cancer. 2015;112:1435-44.
68. Cohen HJ, Feussner JR, Weinberger M, et al. A controlled trial of inpatient and outpatient geriatric evaluation and management. N Engl J Med. 2002;346:905-12.
69. Power DG, Lichtman SM. Chemotherapy for the elderly patient with colorectal cancer. Cancer J. 2010;16:241-52.
70. Bamias A, Lainakis G, Kastritis E, et al. Biweekly carboplatin/gemcitabine in patients with advanced urothelial cancer who are unfit for cisplatin-based chemotherapy: report of efficacy, quality of life and geriatric assessment. Oncology. 2007;73:290-7.