A Novel Combination Immunotherapy Approach for Neuroendocrine Tumors
ONCOLOGY recently spoke with Dr. Sandip Patel about a potential novel therapeutic ap- proach to treating patients with neuroendocrine tumors.
Sandip Patel, MD is a Medical Oncologist and Associate Professor of Medicine at the University of California San Diego School of Medicine in La Jolla, California.

ONCOLOGY recently spoke with Dr. Sandip Patel about a potential novel therapeutic approach to treating patients with neuroendocrine tumors. Dr. Patel is an associate professor of medicine at the University of California San Diego School of Medicine in La Jolla, California. He is also a medical oncologist who specializes in cancer immunotherapy and early-phase immunotherapy clinical trials for patients with various cancer types.
Q: First, how frequently are neuroendocrine tumors diagnosed? What do we know about the biology of these types of tumors?
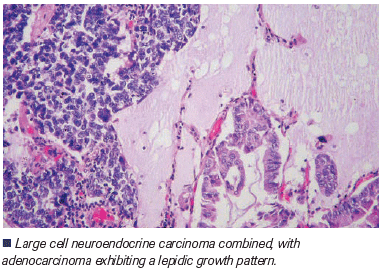
Dr. Patel: Neuroendocrine cancers are a rare, heterogeneous group of tumors that range from low-grade, more indolent tumors to high-grade carcinomas that can be very aggressive. In the United States, the incidence rate of neuroendocrine tumors is approximately 5 cases per 100,000. Since they can manifest in almost any part of the body, clinical trials in this arena have historically been complicated by the varying biologies and sites of origin in which these cancers develop.
Q: Is there an existing standard of care for treating neuroendocrine tumors, or is therapy individualized based on the organ or tissue in which they arise?
Dr. Patel: Broadly speaking, various treatments are used to manage neuroendocrine cancers based on the grade of the tumor and, potentially, the site of origin. For example, pancreatic neuroendocrine tumors are often treated with more targeted approaches, such as agents like sunitinib-an oral, multi-targeted tyrosine kinase inhibitor of vascular endothelial growth factor receptor 1 (VEGFR-1), vascular endothelial growth factor receptor 2 (VEGFR-2), fms-like tyrosine kinase 3 (FLT3), KIT, platelet-derived growth factor receptor à (PDGFRÃ), and platelet-derived growth factor receptor à (PDGFRÃ)-and everolimus, an oral inhibitor of mammalian target of rapamycin (mTOR).
Neuroendocrine cancers that arise in other organs have different therapy options depending on the grade of the tumor. High-grade tumors are often treated with cytotoxic chemotherapy, while low-grade tumors are often treated with somatostatin analogs as well as radio-conjugated somatostatin analogs. So, broadly speaking, the heterogeneity of the tumor type is reflected in the variety of treatment options available for these cancers.
Q: Is there evidence that these tumors respond to immunotherapy?
Dr. Patel: Based on the limited clinical trial data that we have, neuroendocrine cancers do not have a robust response rate to immune checkpoint blockade antibodies. These are agents that activate the immune system via the programmed death 1 (PD-1) and cytotoxic T lymphocyte–associated protein 4 (CTLA-4) pathways. Historically, the response rates to these therapies have been less than 5%.
Q: You are one of the principle investigators of the SWOG 1609 (S1609) trial, also called DART [Dual Anti-CTLA-4 and Anti-PD-1 blockade in Rare Tumors],[1] a study funded by the National Cancer Institute. Can you tell us more about the rationale behind this trial and the study design?
Dr. Patel: S1609 is investigating a dual checkpoint blockade approach that combines ipilimumab, an anti–CTLA-4 immunotherapy antibody, with nivolumab, an anti–PD-1 immunotherapy antibody, across a variety of cancer types in which these agents have not previously been studied. Neuroendocrine tumors are one such tumor type for which limited efficacy data for these immune checkpoint blockade antibodies exist.
I presented the latest data from this trial at the American Association for Cancer Research (AACR) Annual Meeting in April 2019. The most significant finding was that a subset of patients with neuroendocrine tumors, those with high-grade carcinoma, seem to benefit most from dual immunotherapy, with a response rate approaching 44%. Many of those responses, at least initially, appear to be long-lasting and continuous.[1].
Q: What about the toxicity of this immunotherapy combination? How did patients react to this combination therapy?
Dr. Patel: With immune checkpoint blockade antibody treatment, we often see unique immunologic-based toxicities, called immune-related adverse events (IRAEs). In S1609, we utilized a lower dose of ipilimumab than that conventionally utilized to treat patients with metastatic melanoma. Specifically, 1 mg/kg ipilimumab was administered every 6 weeks in combination with nivolumab at a fixed dose every 2 weeks. No fatal IRAEs occurred in this cohort, and there was no evidence of pneumonitis. In addition, the rate of high-grade colitis-one of the most concerning side effects seen with this combination therapy-was 6%. So, overall, the toxicity profile is manageable. Patients, particularly those who continue to respond to therapy, can continue to derive benefit without increasing their toxicity burden.
Q: What is the status of this cohort? How long are the patients being treated and followed up, and when will the next update be?
Dr. Patel: Currently, patients in the neuroendocrine cohort of S1609 continue to receive treatment as long as they derive clinical benefit, do not experience major toxicity, and wish to continue on this study. We scan the study participants every few months, so we plan to update the data at least annually. In particular, we’re interested in investigating the patients with high-grade neuroendocrine carcinoma, given that this is the cohort in which we saw responses.
Q: What have you and your colleagues learned about treating neuroendocrine tumors with immunotherapy? Based on S1609 and other studies, what do we now know about combination treatment with an anti-PD1 and anti-CTLA4 immune checkpoint antibody, and what’s next?
Dr. Patel: To date, neuroendocrine carcinoma clinical trials have faced the same issues that clinical trials for rare cancers and particularly immunotherapy have encountered. Historically, these studies were not done because of the heterogeneity, either related to their tumors or to the neuroendocrine cancer, which is a subset of a rare tumor that has heterogeneity itself. The potential that high-grade neuroendocrine carcinoma has, however, is that it is uniquely sensitive to immune checkpoint blockade, regardless of the organ in which the cancer develops. This may present a development strategy for us to help treat these patients more broadly, regardless of where the cancer begins.
Looking forward, I think that beyond just identifying patients with high-grade neuroendocrine carcinoma who will benefit from dual immune checkpoint blockade, we will focus on why these patients appear to be more responsive to therapy. Is the response related to a specific biomarker, tumor mutational burden, the programmed death ligand 1 marker through an immunohistochemistry test, or to a biomarker we don’t know about yet? If that is the case, have we potentially found something biologically relevant that may be present in other tumor types and help us best select the patients who can benefit from these therapies? So, these are the kinds of translational analyses on patient tissue and blood samples that we will be doing for patients on this cohort, but also more broadly of all of the patients who are part of the S1609 trial.
Q: What major questions remain regarding the potential of immunotherapy for treating neuroendocrine tumors?
Dr. Patel: Given that immune checkpoint blockade has not achieved such a strong response in neuroendocrine cancers in the past, we need to confirm our finding that high-grade neuroendocrine carcinoma patients uniquely confer benefit to dual immune checkpoint blockade. That said, our results-particularly the results we saw for combination therapy with ipilimumab plus nivolumab for high-grade neuroendocrine carcinoma-may be uncovering new biology. If so, what we discover will help us treat not only patients with neuroendocrine cancers, but also patients with other cancer types, once we can figure out the pertinent biomarker that helps drive the response to immunotherapy.
Q: Is there anything else you’d like to add about the uniqueness of treating patients with neuroendocrine cancers?
Dr. Patel: Another reason it has been difficult to conduct studies of rare tumors, including neuroendocrine tumors, is because they often cut across histologies or specialties or even subspecialties within oncology. So, the idea that patients with high-grade neuroendocrine carcinoma appear to benefit from combination immunotherapy, regardless of where the cancer initially developed, is interesting. It provides us with the opportunity to understand the biology and how to best treat these patients, potentially with a biomarker-selected strategy; this may be as simple as factoring in the grade of the tumor, but is likely more nuanced and related to actual immunobiology.
We are particularly interested in sharing this part of the translational analysis. The knowledge we gain may aid in guiding the discovery of new biomarkers and in finding patients with other cancer types who may benefit. Further, it will help us select for patients with neuroendocrine carcinoma who will benefit from this combination therapy, above and beyond just selecting patients based on the grade of their tumors.
Financial Disclosure: DART is funded by the National Institutes of Health through National Cancer Institute grant awards CA180888, CA180819, CA180821, and CA180820 and in part by Bristol-Myers Squibb. Dr. Patel has served in a consulting or advisory position for AstraZeneca, Bristol-Myers Squibb, and Tempus.
Key Question
At the AACR 2019 Annual Meeting, you also presented data from this trial on the cohort of patients with nonpancreatic neuroendocrine tumors. Can you tell us about your findings and what the efficacy results show so far?
Dr. Patel: The cohort data presented at AACR included patients with both low-grade and high-grade nonpancreatic neuroendocrine cancers who were treated with immune checkpoint blockade. We found a 44% overall response rate among patients with high-grade carcinoma compared with a 0% response rate in patients with low- to intermediate-grade tumors.[1] Based on these findings, we are currently planning a new cohort study as part of S1609 that is dedicated to patients with high-grade neuroendocrine carcinoma to evaluate this effect further.
PERSPECTIVE
Medical Community Must Support More Research
Philip Philip, MD, PhD, FRCP
The management of patients with high-grade neuroendocrine tumors (NETs) remains challenging despite the significant objective responses seen with frontline therapy of platinum-based chemotherapy and etoposide combinations. Historically, there has been a paucity of clinical investigation of patients with neuroendocrine tumors partly because of the low incidence of this tumor type. It is therefore very encouraging that there may be another option for those patients based on the preliminary results from the DART study. The objective response rate of 44% and the durable responses seen in the DART study are intriguing because to date such a response rate has not been seen beyond the response rates using etoposide and platinum combination therapy in treatment naïve patients. However, we need more mature data from the DART study, and particularly overall survival data. Additionally, one cannot be certain at this time whether a dual blockade of PD-1 or PD-L1 inhibition combined with inhibition of CTLA-4 is necessarily better in terms of efficacy and safe compared to the use of a PD-1 or PD-L1 inhibitor alone. In a disease such as high-grade NET it may also be interesting to see whether the addition of immunotherapy to the frontline cytotoxic therapy will produce a better outcome compared to cytotoxic therapy alone. Another attractive option would be to use immunotherapy as a maintenance treatment following the conclusion of initial successful induction chemotherapy. The use of the DART regimen in the frontline setting without chemotherapy will not be an option because of the objective response rate of 44% that is inferior to what we get with the currently used combination therapy. In patients with high grade NET who often are symptomatic there is a need to achieve a timely and effective cytoreduction.
Results of the DART study also support what we know about the microenvironment in high-grade NETs which is that the microenvironment is very different compared to that in well-differentiated neuroendocrine tumors and that the microenvironment within NETs is more conducive to a response to immunotherapy. These data also are consistent with the benefits of immune checkpoint inhibitors in patients with small cell lung cancer, a biologically related disease. It would be interesting to see whether immunotherapy is also beneficial for grade 3 well differentiated NETs, although my guess is that it is not going to be as effective as in patients poorly differentiated NETs. There is a need to support future studies in this disease realizing the rarity of high-grade NETs. Any opportunity for a national trial, especially a prospective, randomized one, must be strongly supported by the oncology community. Research on how best to select patients for such therapy is also needed.
Financial Disclosure:Dr. Philip has received research funding, and/or speaker or consultant fees from AAA, Merck, and BMS.
Dr. Phillip is leader of the Multidisciplinary Team for Gastrointestinal Oncology at the Barbara Ann Karmanos Cancer Institute, and Professor at Wayne State University School of Medicine, Detroit, Michigan.
References:
1. Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063-72.
2. National Cancer Institute. targeted therapies sunitinib and everolimus improve survival for patients with rare type of pancreatic cancer. Available at: https://www.cancer.gov/types/pancreatic/research/neuroendocrine-sunitinib-everolimus Accessed November 5, 2019.
3. Weber MM, Fottner C. Immune checkpoint inhibitors in the treatment of patients with neuroendocrine neoplasia. Oncol Res Treat. 2018;41:306-12.
4. Patel SP, Othus M, Chae YK, et al. SWOG 1609 (DART): A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors. J Clin Oncol. 2019;15(suppl):abstr TPS2658.
5. Thompson JA, Schneider BJ, Brahmer J, et al. management of immunotherapy-related toxicities, version 1.2019. J Natl Compr Canc Netw. 2019;17:255-89.
How Supportive Care Methods Can Improve Oncology Outcomes
Experts discussed supportive care and why it should be integrated into standard oncology care.