Capecitabine Plus Irinotecan Tested as Colorectal Cancer Regimen
BIRMINGHAM, England-Combining capecitabine (Xeloda) and irinotecan (Camptosar) is feasible at doses effective for treating colorectal cancer, according to David Kerr, MD, DSc. He reviewed early capecitabine/irinotecan trials and said that the combination should be evaluated in phase III trials against metastatic cancer, as adjuvant treatment, and using oral formulations of both drugs. Dr. Kerr is professor of clinical oncology at the CRC Institute for Cancer Studies, Birmingham, England.
BIRMINGHAM, EnglandCombining capecitabine (Xeloda) and irinotecan (Camptosar) is feasible at doses effective for treating colorectal cancer, according to David Kerr, MD, DSc. He reviewed early capecitabine/irinotecan trials and said that the combination should be evaluated in phase III trials against metastatic cancer, as adjuvant treatment, and using oral formulations of both drugs. Dr. Kerr is professor of clinical oncology at the CRC Institute for Cancer Studies, Birmingham, England.
Dr. Kerr said that the combination is attractive because the two drugs have different molecular mechanisms of action, both are active in colorectal cancer, and sequential combination of low doses of irinotecan and capecitabine has been "highly curative" in preclinical studies. Irinotecan also has activity in tumors resistant to fluoropyrimidines.
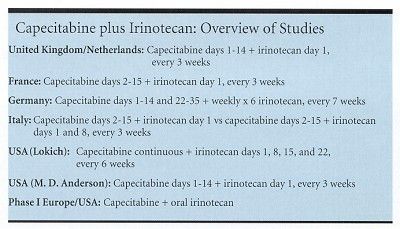
Dr. Kerr reviewed phase I/II studies done by several groups in the United Kingdom, the Netherlands, France, Germany, Italy, and the United States. "The ongoing US/European phase I trial is important because all of us are interested in what comes of a truly oral combination," Dr. Kerr said.
Different Dose Levels
The maximum tolerated dose (MTD) in the UK/NL study was capecitabine 1,250 mg/m² twice daily, days 1 to 14, and irinotecan 300 mg/m² as a 30-minute IV infusion on day 1. Dr. Kerr said that patients are continuing at dose level 4 to confirm the recommended dose. "Preliminary efficacy is promising, with responses at every dose level," he said.
Toxicity at dose level 3 caused German researchers to back down a dose level to capecitabine 1,000 mg/m² twice daily for days 1 to 14 and 22 to 35 every 7 weeks, and irinotecan 70 mg/m² on a weekly × 6 schedule every 7 weeks. Trying a fractionated irinotecan schedule in an attempt to reduce the incidence of severe alopecia proved to be a successful strategy. The overall response rate was 45%.
Dose levels in the Italian phase II study appeared to be "plucked out of the air," according to Dr. Kerr. Grade 3/4 diarrhea, hand-foot syndrome, and neutropenia were seen in 15% to 20% of the first 47 patients, so the study continued with reduced doses (capecitabine 1,000 mg/m² twice daily, days 2 to 14, and irinotecan as a 90-minute IV infusion either 240 mg/m² on day 1 or 120 mg/m² on days 1 and 8, repeated every 21 days. The 34 evaluable patients had an overall response rate of 65%.
"Taken together, these trials suggest that combination capecitabine/irinotecan regimens are feasible at effective doses and that toxicity becomes an issue at irinotecan doses of 250 mg/m²," Dr. Kerr said. Phase III capecitabine/irinotecan studies in advanced metastatic cancer and as adjuvant therapy are planned, probably with irinotecan at 250 mg/m² and capecitabine at 2,000 mg/m² and a cycle that repeats every 3 weeks. Dr. Kerr added that researchers would like to be able to collect basic genetic polymorphism information to help determine which patients are responding to which regimens.