Changing the Paradigm
ONCOLOGY recently sat down with Kenneth C. Anderson, MD, to discuss the current trends in multiple myeloma treatment, and the explosion of novel therapies that are paving the way to better and more durable outcomes and allowing patients to live longer and more meaningful lives.
Dr. Anderson is the program director of the Jerome Lipper Multiple Myeloma Center and LeBow Institute for Myeloma Therapeutics at Dana-Farber Cancer Institute.
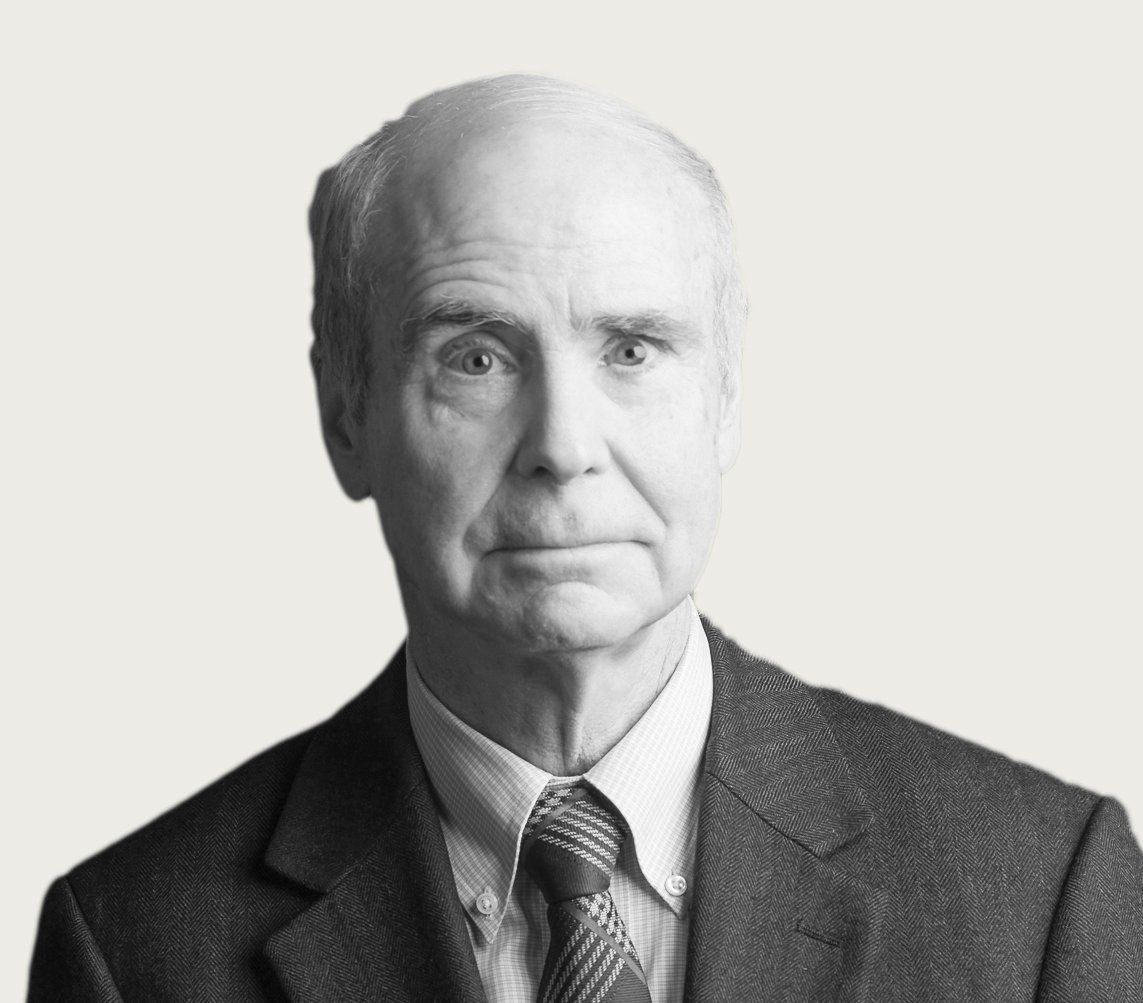
Thirty years ago, patients with multiple myeloma faced a poor prognosis, with 5-year survival rates of approximately 25%. With the development of immunotherapy and targeted agents, that number has now almost doubled. ONCOLOGY recently sat down with Kenneth C. Anderson, MD, to discuss the current trends in multiple myeloma treatment, and the explosion of novel therapies that are paving the way to better and more durable outcomes and allowing patients to live longer and more meaningful lives. While the recent progress has undoubtedly changed the treatment landscape for multiple myeloma, the future, Anderson says, is even brighter.
Q: Multiple myeloma seems to be one of the fastest changing realms of cancer care. What would you say are the major trends in multiple myeloma treatment over the past year or so?
DR.ANDERSON: There has been very rapid progress, both in the targeted therapy and immune therapy areas. A targeted therapy, for example, such as venetoclax (Venclexta) is very effective in 11;14 translocation or high B-cell lymphoma 2 (BCL-2)-expressing myeloma. On the immune side, there are B-cell maturation antigen (BCMA)-directed immunotoxins, bispecific T-cell engagers (BiTEs), and chimeric antigen receptor (CAR) T cells, all of which are looking very promising in clinical trials. So, rapid progress is being made in…the targeted therapy area and [with] immune therapies.
Q: There is also a fair amount of clinical work going on with combinations, not just individual agents. What interests you there?
DR.ANDERSON: So, there is continued progress in combinations. Our progress to date has been related to developing new classes of drugs and then combining them based on preclinical rationale, suggesting that they are additive or synergistic. So, for example, in newly diagnosed patients, lenalidomide (Revlimid)/bortezomib (Velcade)/dexamethasone (RVd) were combined and are used broadly [in]… patients [with myeloma] and achieve a very high rate of response and extent of response.
The monoclonal antibodies, daratumumab (Darzalex) and elotuzumab (Empliciti) (especially daratumumab), now have been added to RVd and at this [past] American Society of Hematology (ASH) [Annual Meeting and Exposition in December 2019], RVd/daratumumab or carfilzomib (Kyprolis)/lenalidomide (Revlimid)/dexamethasone (KRd)/daratumumab were shown to achieve …[an] even deeper or higher extent of response, including a high frequency of minimal residual disease (MRD)-negative responses. So, adding an antibody to RVd or KRd is increasing the extent of response.
In the relapsed/refractory setting, new regimens are also based on combination approaches. At the ASH annual meeting, for example, carfilzomib (Kyprolis)/dexamethasone/daratumumab were compared with carfilzomib (Kyprolis)/dexamethasone, and the triplet was found to be superior in terms of treatment for relapsed myeloma. So, in newly diagnosed [patients] and in[those who have] relapsed , novel combinations are showing more efficacy.
Q: What studies that have yet to report results are folks in the research industry most excited about?
DR.ANDERSON: I think in terms of the combination approaches, the Intergroupe Francophone Myelome (IFM)/Dana-Farber Cancer Institute (DFCI) trial, which is RVd in newly diagnosed myeloma transplant candidates…as initial therapy, and then randomization… to… early high-dose melphalan (Alkeran) in stem cell transplant versus not. This trial has been going on since 2009 and [it] is asking the question as to the added value of a stem cell transplant in the era of combination novel therapies. So that is one trial that we are really anticipating and excited about the results.
In the relapsed setting, I will cite 2 examples [with results] coming out that hopefully will change practice. There is a new CD38 antibody called isatuximab which has some characteristics similar to daratumumab but…[it] is qualitatively different. A large randomized phase [III] trial of isatuximab with pomalidomide (Pomalyst)/dexamethasone versus pomalidomide/dexamethasone [alone] is fully enrolled and it is expected that the results of this trial will provide the framework for its FDA approval to treat relapsed myeloma. A second example would be the trials of 11;14 translocation myeloma or myeloma that expresses high levels of BCL-2.
A randomized study called the BELLINI trial has compared venetoclax/bortezomib (Velcade)/dexamethasone with bortezomib (Velcade)/dexamethasone and shown that the benefits are primarily in those patients who have the 11;14 translocation or express high levels of BCL-2, whereas other patients do not similarly benefit. Those would be among the most exciting short-term trials. I would also say that the excitement is in the immune trials,…in 3 areas. There is the BCMA immunotoxin from GlaxoSmithKline and clinical trials of this immunotoxin are showing activity in relapsed multiple myeloma with significant prolongation of progression-free survival that should provide the benefit for its FDA approval.
There are now many BiTEs. Early data presented at the [recent] ASH [meeting] showed that once the correct dose was defined, significant responses in terms of high rates of response and high rates of MRD negativity were achieved. And thirdly, the clinical trials of CAR T-cell [therapy] are numerous and very promising. I think a summary in myeloma would be that the responses are in far-advanced myeloma and extremely deep. Often, MRD-negative complete responses are achieved in spite of multiple prior therapy. The safety [of CART T-cell therapy] is being improved, [as a] decreased [incidence] of serious cytokine release syndrome (CRS) [has been] observed. What remains as an obstacle is the durability, as progression-free survival on average is still around 18 months.
Q: Of the CAR T-cell therapy trials, which is furthest along? Is this something we would expect to see become a standard of care-at least in sort of heavily pretreated myeloma-in the near future?
DR.ANDERSON: I think that the furthest along in the CAR T-cell [therapy] area are the bb2121 CAR T-cell approaches. The response rates are very high in spite of multiple lines of prior therapy and I would anticipate that [bb2121] would be approved later in 2020 or early in 2021. Multiple other trials are trying to, if you will, improve upon the durability and efficacy of CAR T-cell therapy. So, for example, the bb21217 concept is [manufacturing] CAR T cells in the presence of a phosphoinositide-3 kinase inhibitor to select for early lineage memory CAR T cells. Early data suggest that you can detect memory CAR T cells in patients after treatment.
There are experiments utilizing combinations of CD4- and CD8-positive CAR T cells. There are CAR T cells that have been modified so they bind to BCMA in 2 different domains, the so-called bivalent CAR T cells. The initial experience was in China and very encouraging, showing that fewer CAR T cells are needed and high rates of response and extent of response [were] observed. Now in America, the same bivalent BCMA vector is used, and [results from] the CARTITUDE-1 trial [were] reported at the [recent ASH meeting]. Very high rates of response, and extent of response, including MRD negativity were observed, but the follow-up is short and the durability of those responses remains to be seen.
Q: You talked about the incidence of CRS going down. Was that particularly high in the initial trials of CAR T-cell therapy? And what they have been doing to get it down?
DR.ANDERSON: Well, I think the severe CRS was observed primarily in the earliest studies. And subsequent, there has been [a] marked increase in [the] understanding and…recognition of CRS, and…in its treatment-such that [the] tocilizumab (Actemra) antibody directed at interleukin-6 is used often and early and can in large part aggregate severe CRS.
Q: Is there work underway to move the use of CAR T-cell therapy earlier in the process as frontline treatment or at least in the less heavily pretreated patients?
DR.ANDERSON: Yes, there is. As with our other novel drug or immune approaches, CAR T-cell [therapy] is now being first tested in far advanced patients with relapsed/refractory disease. Having established efficacy and safety in that setting, [CAR T cells] are now being tested earlier in the disease course. For example, in patients who have high-risk, genetically high-risk multiple myeloma, such as [those with a 17p delet[ion], CAR T cells are being utilized at the time of first relapse…, so relatively early in the disease course.
Q: Is there hope that eventually CAR T-cell therapy might be a replacement for traditional transplantation?
DR.ANDERSON: Yes, I think there are trials that are planned and will start in the not [so] distant future that will compare stem cell transplant[ation] with CAR T-cell [therapy], probably starting first in the high-risk genetically defined [patients with] 17p delet[ion]. We need to remember [that transplantation has been] well established…for decades in terms of achieving [a] high extent and frequency of response [and] progression-free [survival] and in many studies, [an] overall survival advantage. I do think there will soon be comparative randomized trials of conventional stem cell transplantation versus CAR T-cell [therapy], and we do need that objective data before we make any paradigm shifts in terms of myeloma therapy.
Q: The other immunotherapies you discussed differ from the traditional checkpoint inhibitors that oncologists are most familiar with. Can you talk about how they work? What are they doing that allows the immune system to better attack myeloma?
DR.ANDERSON: Well, the BCMA immunotoxin that is currently moving towards FDA approval has 2 mechanisms. It has immune effects from a BCMA antibody which include antibody-dependent cellular cytotoxicity and complement-dependent cytotoxicity. It also delivers to the BCMA-positive myeloma an auristatin immunotoxin as a second mechanism of myeloma killing. The second or next class of drugs are called BiTEs, and they…have 2 antibody-binding domains. They bind on the one hand to BCMA-positive multiple myeloma cells and on the other to CD3 on the surface of T immune cells, thereby bringing the immune cells in proximity to the myeloma cells. As in leukemia and lymphoma, early data in myeloma suggest that you can have [greater] potency, more selectivity, and perhaps a better therapeutic index by localizing the immune response in the microenvironment of the tumor and potentially avoid more systemic side effects.
I think people understand how [CAR T-cell therapy] work[s], but I will just mention [that] the T cells are harvested from patients with myeloma, transfected usually with a lentiviral vector that allows for their binding to BCMA-positive myeloma cells, [which] activates their T-cell receptor, and usually has a costimulatory molecule (4-1BB or CD28). These transfected BCMA-targeting autologous T cells, which are activated…[and]then expanded ex vivo or in the laboratory with CD3/CD28 beads into large numbers. These autologous cells are then transfused back to patients, as I like to say, [to] their own immune army. And, as I mentioned already, very impressive extent and frequency of responses are observed.
Q: What is driving these new trials? Is it a better understanding of the underlying biology of the myeloma?
DR.ANDERSON: I think it is a combination [of things]. Certainly, the single agents and combination therapies are being informed by preclinical science, both in the laboratory and in animal models, which suggest cytotoxicity directed at myeloma cells that can be enhanced or…synergistic effects when used in combination. There are also observations at the bedside that are then brought back to the laboratory, back to the bench, and result in further experimentation and improvement in some strategies that can go back to the clinic. So, it is [that] bed-to-bench-to-bedside iteration that leads to improved therapies or improved combination therapies and improved efficacy.
Q: What are the big things we have learned about the biology of multiple myeloma in the past couple of years?
DR.ANDERSON: Well, we have known for many years that myeloma evolves from monoclonal gammopathy of undetermined significance (MGUS) to a stage called smoldering multiple myeloma and then to active multiple myeloma disease. Traditionally, we have only treated myeloma when complications develop, such as hypercalcemia, renal disease, anemia, or bone disease. Starting in 2016, because we have very effective therapies for myeloma that are well tolerated, we have now redefined smoldering multiple myeloma and treat some of those affected patients before they develop [hypercalcemia], kidney [disease], anemia, or bone disease. In particular, even patients who do not have those end-organ sequalae are treated if they have more than 60% plasma cells,…bone disease on sensitive imaging, or…a kappa lambda ratio more than 100-fold abnormal. In these patients, we hope by treating early we can prevent or delay the development of those complications. That is a major clinical advance.
In terms of the biology of the progression from MGUS to smoldering myeloma to multiple myeloma, recent studies have characterized the genetic progression of disease and shown that the majority of changes genetically are already present at the MGUS stage. Patients who progress rapidly to myeloma are those who have expansion of an abnormal genetic clone that was already there at time of diagnosis. Those patients who take a longer time to progress have what we call clonal evolution where there is genetic, if you will, changes that occur in the myeloma clone that ultimately correlate with progression.
The major point here is that since the majority of genetic changes are present very early, many laboratories and investigators have turned their attention to the bone marrow microenvironment. Changes in the bone marrow milieu,…accessory cells in the bone marrow and the patient’s immune cells in the bone marrow,…actually correlate or are associated with progression of disease. In other words, if the majority of genetic changes are already there very early, the progression may very likely be due to changes in the patient’s bone marrow microenvironment, the accessory cells there, and especially the patient’s autologous immune system.
Q: You talked about specific mutations appearing to make particular treatments work more effectively. How many patients with multiple myeloma right now have a mutation that would drive treatment? And what efforts are underway to sort of segment people a little better to see what is going to work for whom?
DR.ANDERSON: There has been significant progress in terms of the genetic profiling of myeloma for use at [the] time of diagnosis and for prognosis. We have progressed from fluorescent in situ hybridization to gene sequencing of patients’ multiple myeloma cells. To date,…the only precision medicine in multiple myeloma is venetoclax alone or together with a proteasome inhibitor in patients who have 11;14 translocation or high BCL-2 expression. That population ranges somewhere between 30% and 40% of patients [with myeloma]. I and others have sequenced large numbers of patients with myeloma…to subset them, and they are based on bulk RNA characterization. There are at least 11 subgroups of multiple myeloma based on DNA sequencing. There are large numbers of mutations, some of which appear to be driver mutations.
For example, RAS or KRAS are the most commonly mutated genes in myeloma, and there have been early attempts to block the RAS/rapidly accelerated fibrosarcoma/mitogen-activated protein kinase signaling pathway using MEK inhibitors or extracellular signal-regulated kinases inhibitors. These treatments have achieved responses that were only transient. Combination targeted therapies are now being employed. Clinical trials are being done, such as the MyDRUG (Myeloma–Developing Regimens Using Genomics) umbrella trial, to try to treat patients with relapsed myeloma with precision medicine.
I will mention that in this trial, patients’ myeloma, when it relapses, is being sequenced. These patients are then being treated with an active regimen of the proteasome inhibitor, ixazomib (Ninlaro), and the immunomodulatory drug, pomalidomide, to which is added a targeted therapy based upon the mutations that are identified. The…MyDRUG umbrella trial will define whether the targeted therapy actually depletes the mutated myeloma clone. And, if it does, this will be a hypothesis or a new lead to be tested further in subsequent clinical trials.
But, in summary, myeloma is extremely heterogeneous right at diagnosis. There is continual ongoing DNA damage and genomic evolution as the disease progresses. And, as of today, the only real true precision medicine in myeloma would be venetoclax-containing regimens in the 11;14 translocation or high BCL-2-expressing myeloma subset.
Q: Which investigations have you been actively involved with?
DR.ANDERSON: Our center has been involved in the preclinical evaluation and clinical trial evaluation of all of [these] advances. And we have been blessed in multiple myeloma to have 26 FDA approvals [to date] which have incorporated novel agents, and our center has been actively involved in the preclinical and clinical development of 22 of those new advances.
Q: Of all the clinical trials that you have been involved with, are there 3 or 4 that you would consider to be your “greatest hits?”
DR.ANDERSON: One is the trials of proteasome inhibitors, in particular bortezomib (Velcade) in the early 2000s, that achieved remarkable responses in far advanced relapsed/refractory myeloma, ultimately leading to FDA approval. We similarly participated in the preclinical and clinical development of lenalidomide, which…was FDA approved, first in relapsed myeloma and then [as part of] combination [therapy].
So, we did clinical trials…of the combin[ation of] lenalidomide (Revlimid) with bortezomib (Velcade) and dexamethasone based on preclinical studies, and this RVd regimen achieved high response rates and extent of response and is now used all over the world as initial therapy in myeloma.
The most important trial I think that is not yet mature is the DFCI/IFM trial, which is…RVd given to newly diagnosed transplant candidates, with…randomization to high-dose melphalan and stem cell transplantation or not, in each case followed by lenalidomide maintenance. This is a landmark trial in myeloma as it will define the utility of high-dose melphalan and stem cell transplantation in the era of novel combination targeted agents.
Q: Which investigational accomplishments from your career are you most proud of?
DR.ANDERSON: I think that when I began studying multiple myeloma back in the 1970s, the survival of patients was only a few months. And then starting in 1980, I extended my interest to a laboratory interest in multiple myeloma which involves studying not only the myeloma cell but also the microenvironment. The advances came in the 1980s, primarily…high-dose melphalan and autologous stem cell transplantation. The bisphosphonates came [into use] in the early 1990s to avoid the terrible bony complications of myeloma.
But to get to your question, the most exciting accomplishments or progress that I have been associated with has to do with the advances since the late 1980s-novel drug classes that target both the tumor and the microenvironment. And these drugs…are the immunomodulatory drugs, the proteasome inhibitors, [and] monoclonal antibodies. And these advances, these classes of agents used sometimes alone, but much more commonly in scientifically informed combinations, have transformed…outcome[s] in myeloma.
At the present time, for example, novel combination agents are used to treat newly diagnosed myeloma and achieve responses in the overwhelming majority of patients. These combinations of 3 and now 4 agents are so active that we have clinical trials examining whether high-dose melphalan and stem cell transplantation adds [any] value. And novel agents such as lenalidomide and others have been used as maintenance…to transform myeloma into a chronic illness in many cases.
I am most proud of the role that our group and our very large laboratory and clinical effort has played in these advances in drugs targeting the tumor and the microenvironment and in particular, in the transformation of myeloma treatment. It is said that patients’ survival [has] improved at least 3- to 4-fold. That is a conservative estimate because many patients on maintenance therapy truly do have myeloma as a chronic illness and grow old and die of something else.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.