Considerations When Initiating Neratinib for Breast Cancer: How to Prevent and Treat Diarrhea
An oncology pharmacist discusses how to prevent and treat diarrhea in patients taking neratinib for breast cancer.
Oncology (Williston Park). 33(6):232-4.

Meagan S. Barbee, PharmD, BCOP

Table 1. Practical Considerations for Neratinib Use
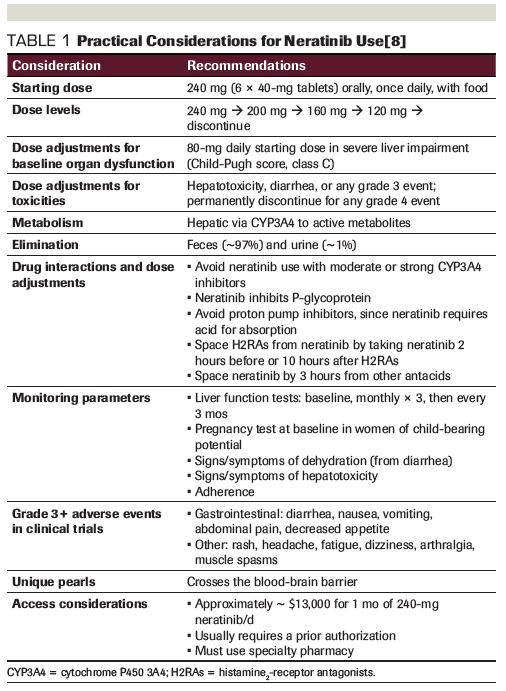
Table 2. Prevention of Neratinib-Induced Diarrhea
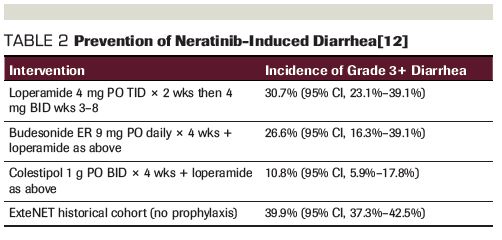
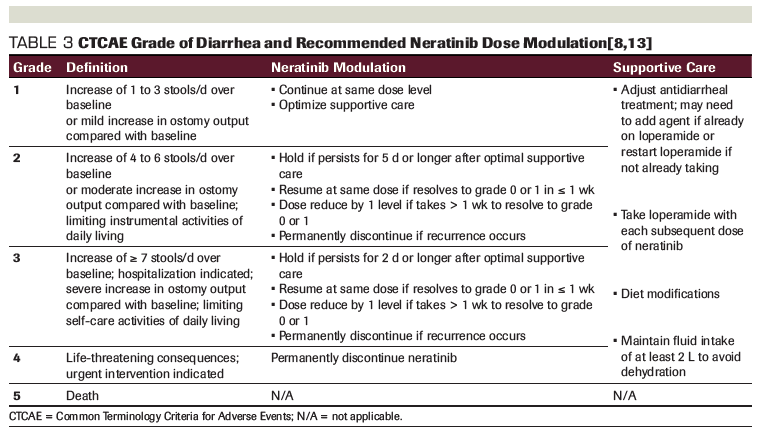
Table 3. CTCAE Grade of Diarrhea and Recommended Neratinib Dose Modulation
The adjuvant treatment landscape for breast cancer has changed drastically in recent years.[1] For patients with hormone receptor (HR)-positive disease, data suggest that 10 years of hormonal therapy is better than 5 years,[2-4] and that high-risk patients who are premenopausal should receive ovarian suppression and an aromatase inhibitor instead of tamoxifen or tamoxifen with ovarian suppression.[5] Moreover, patients whose Oncotype DX score is less than 26 are unlikely to benefit from chemotherapy based on results from the TAILORx study.[6] In HER2-negative patients who received neoadjuvant therapy but did not achieve a pathologic complete response, adjuvant capecitabine for 6 to 8 cycles (before endocrine therapy in HR-positive patients) should be considered, according to results of the CREATE-X study.[7] Lastly, neratinib was approved by the US Food and Drug Administration (FDA) in 2017 for the extended adjuvant treatment of HER2-positive breast cancer per the results of the ExteNET trial.[8-10]
In the ExteNET trial, patients with early HER2-positive disease who underwent previous chemotherapy received 1 year of extended adjuvant therapy with once-daily oral neratinib 240 mg following a year of standard-of-care adjuvant trastuzumab. The study was eventually amended to include only higher-risk patients (those with node-positive disease, stages II to III) who were no more than 1 year from their last dose of adjuvant trastuzumab and had no evidence of recurrence. In patients who were HR positive (57% of the overall population), neratinib was given concurrently with adjuvant endocrine therapy. Patients with clinically significant cardiac, gastrointestinal, or psychiatric comorbidities and those unable to swallow pills were excluded from the trial. Results showed that 1 year of adjuvant neratinib significantly improved the 2-year invasive disease–free survival rate compared with placebo (93.9% vs 91.3%, respectively; stratified hazard ratio, 0.67; 95% CI, 0.50–0.91; P = .0017). However, the clinical benefit was not preserved in the subgroup of patients who were HR negative (hazard ratio, 0.93; 95% CI, 0.60–1.43; P = .74, pinteraction = .54).[9] Primary endpoint results were preserved in a 5-year follow-up report.[10]
Neratinib is an irreversible tyrosine kinase inhibitor of HER1 (ErbB1, epidermal growth factor receptor [EGFR]), HER2 (ErbB2), and HER4 (ErbB4).[8] Practical considerations for neratinib use are listed in Table 1. Neratinib is associated with severe skin rash, interstitial lung disease, hepatotoxicity, and pneumonitis. The most commonly reported adverse event and dose-limiting toxicity of neratinib is diarrhea.[8-10] In the ExteNET trial, 41% of patients experienced a grade 3 or higher diarrhea event, with a median time to onset of 8 days and a median duration of 5 days. Diarrhea of any grade was experienced by 95% of patients in the trial, and led to dose reductions in 26% and study discontinuations in 17% of patients in the neratinib arm, resulting in an overall median relative dose intensity of 82% for neratinib (98% for placebo). Twenty patients (1%) were hospitalized as a result of neratinib-induced diarrhea. Negative changes in quality of life on neratinib were reported at 1 month, though scores recovered to baseline soon after, and the effects of diarrhea on this change were not studied.[9] However, diarrhea can have a notable effect on performance status and the ability to perform activities, resulting in social isolation, time off work, relationship difficulties, and psychological distress.[11]
The mechanism of neratinib-induced diarrhea is likely due to its effect on EGFR, similar to that of erlotinib; EGFR mediates calcium-dependent chloride transport, and blocking EGFR can subsequently induce secretory diarrhea.[11] Because of the significant incidence of diarrhea with use of neratinib, the original FDA labeling for the approval of neratinib included a recommended prophylaxis of loperamide scheduled for 2 cycles (2 months total), beginning with the first dose, and continuing as needed thereafter.[8] Optimal prevention of neratinib-induced diarrhea is being studied in the phase II CONTROL trial.[12] Early findings (Table 2) suggest that adding colestipol to loperamide beginning with the first dose of neratinib results in the greatest reduction of grade 3 or higher diarrhea incidence (primary endpoint) and severity compared with what was seen in the ExteNET trial.
Providers should be aware of the risk of diarrhea with neratinib initiation and proactively prescribe colestipol 1 g PO BID × 4 weeks in conjunction with loperamide 4 mg PO TID × 2 weeks, 4 mg BID for weeks 3 to 8, and then as needed thereafter. If this approach is unsuccessful, dose modulation of neratinib should occur, according to Common Terminology Criteria for Adverse Events (CTCAE) grade (Table 3). Other agents could be employed in the treatment of diarrhea, should it continue, and may include: codeine, octreotide, budesonide, and antibiotics.[11] Supportive care should be maximized at the onset of any grade of diarrhea. Neratinib should be held for complicated diarrhea that includes features of dehydration, fever, hypotension, renal failure, or neutropenia (absolute neutrophil count < 1,000/mm3). If constipation is experienced, the dose of loperamide should first be decreased or the schedule altered to be less frequent, but not initially abandoned. Neratinib should be discontinued if the toxicity does not recover to ≤ grade 1, if the toxicity results in a treatment delay of more than 3 weeks, or in patients unable to tolerate 120 mg in the absence of baseline organ dysfunction.[8]
Patients should be monitored for compliance to neratinib and the prophylactic antidiarrheal regimen to help preserve adherence and limit unnecessary and preventable dose reductions or neratinib failures. Ongoing drug interaction assessments should be performed at each physician visit to screen for medications that can increase the AUC of neratinib via cytochrome P450 (CYP) inhibition, thus perpetuating diarrhea, as well as for concomitant medications that are independently associated with diarrhea. Patients should be counseled to refrain from over-the-counter stool softeners and laxatives when initiating neratinib therapy.
While patients have received a marginal clinical benefit from extended adjuvant therapy with neratinib in the curative-intent setting, it is likely that utilization of neratinib will expand to the HER2-positive metastatic setting, particularly in patients with brain metastases. In the future, preserving high doses of neratinib to maximize central nervous system concentration in patients with brain metastases who have few alternative options for therapy will rely on adequately preventing and controlling major toxicities, namely diarrhea. While use in the metastatic setting is currently off-label, and it is currently unknown whether adherence or dose preservation affect disease-free survival in the curative-intent setting, providers should still aim to prevent diarrhea in patients receiving neratinib to optimize therapy and maintain a good quality of life.
Financial Disclosure:Dr. Barbee has no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Denduluri N, Chavez-MacGregor M, Telli ML, et al. Selection of optimal adjuvant chemotherapy and targeted therapy for early breast cancer: ASCO Clinical Practice Guidelines focused update. J Clin Oncol. 2018;36:2433-43.
2. Goss PE, Ingle JN, Pritchard KI, et al. Extending aromatase-inhibitor adjuvant therapy to 10 years. N Engl J Med. 2016;375:209-19.
3. Blok EJ, Kroep JR, Meershoek-Klein Kranenbarg E, et al. Optimal duration of extended adjuvant endocrine therapy for early breast cancer: results of the IDEAL trial (BOOG 2006-05). J Natl Cancer Inst. 2018;110:40-8.
4. Goldvaser H, Barnes TA, Seruga B, et al. Toxicity of extended adjuvant therapy with aromatase inhibitors in early breast cancer: a systematic review and meta-analysis. J Natl Cancer Inst. 2018;110:31-9.
5. Francis PA, Pagani O, Flemin GF, et al. Tailoring adjuvant endocrine therapy for premenopausal breast cancer. 2018;379:122-37.
6. Sparano JA, Gray RJ, Makower DF, et al. Adjuvant chemotherapy guided by a 21-gene expression assay in breast cancer. N Engl J Med. 2018;379:111-21.
7. Masuda N, Lee SJ, Ohtani S, et al. Adjuvant capecitabine for breast cancer after preoperative chemotherapy. N Engl J Med. 2017;376:2147-59.
8. Nerlynx (neratinib) [prescribing information]. Los Angeles, CA: Puma Biotechnology, Inc; June 2018. https://nerlynx.com/pdf/full-prescribing-information.pdf. Accessed April 2, 2019.
9. Chan A, Delaloge S, Holmes FA, et al. Neratinib after trastuzumab-based adjuvant therapy in patients with HER2-positive breast cancer (ExteNET): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2016;17:367-77.
10. Martin M, Holmes FA, Ejlersten B, et al. Neratinib after trastuzumab-based adjuvant therapy in HER2-positive breast cancer (ExteNET): a 5-year analysis of a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1688-1700.
11. Andreyev J, Ross P, Donnellan C, et al. Guidance on the management of diarrhoea during cancer chemotherapy. Lancet Oncol. 2014;15:e447-e460.
12. Hurvitz S, Chan A, Iannotti N, et al. Effects of adding budesonide or colestipol to loperamide prophylaxis on neratinib-associated diarrhea in patients with HER2+ early-stage breast cancer: the CONTROL trial. Presented at the 40th Annual San Antonio Breast Cancer Symposium (SABCS); Dec 5-9, 2017; San Antonio, TX. Abstract P3-14-01.
13. US Department of Health and Human Services; National Institutes of Health, National Cancer Institute. Common Terminology Criteria for Adverse Events, Version 5.0. November 27, 2107. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf. Accessed April 2, 2019.