Hyperthermia as a Treatment for Bladder Cancer
Modern cancer care is characterized by a focus on organ-sparing multi-modal treatments. In the case of non–muscle-invasive bladder cancer this is particularly true; treatment is focused on reducing the frequency of low-risk recurrences and preventing high-risk progression. Deep regional hyperthermia is an oncologic therapeutic modality that can help achieve these two goals. The combination of hyperthermia with chemotherapy and radiotherapy has improved patient outcomes in several tumor types. In this review, we highlight the biology of therapeutic fever-range hyperthermia, discuss how hyperthermia is administered and dosed, demonstrate how heat can be added to other treatment regimens, and summarize the data supporting the role of hyperthermia in the management of bladder cancer.
Modern cancer care is characterized by a focus on organ-sparing multi-modal treatments. In the case of non–muscle-invasive bladder cancer this is particularly true; treatment is focused on reducing the frequency of low-risk recurrences and preventing high-risk progression. Deep regional hyperthermia is an oncologic therapeutic modality that can help achieve these two goals. The combination of hyperthermia with chemotherapy and radiotherapy has improved patient outcomes in several tumor types. In this review, we highlight the biology of therapeutic fever-range hyperthermia, discuss how hyperthermia is administered and dosed, demonstrate how heat can be added to other treatment regimens, and summarize the data supporting the role of hyperthermia in the management of bladder cancer.
The recognition of a possible therapeutic benefit of local hyperthermia on the biology of cancer cells dates back for many decades.[1,2] In the time since this discovery, the delivery of hyperthermia has evolved, along with the ability to combine it with other treatment modalities; there has also been continuing elucidation of hyperthermia’s many mechanisms of action. Much of the limitation in the use of therapeutic hyperthermia in the treatment of cancer has been due simply to the inability to effectively deliver locoregional hyperthermia to the target tissue and to monitor temperatures as the treatment is given. The recent development of more sophisticated heat delivery systems and cutting edge thermal dose modeling tools has allowed researchers to better direct the energy required to produce hyperthermia to the sites of desired therapeutic effect. Consequently, phase II and III investigations have been conducted and have demonstrated that hyperthermia can benefit patients with certain types of tumors.
In general, hyperthermia is used as either a radiosensitizer or chemosensitizer and has been part of a combined treatment protocol for tumors in superficial locations (eg, melanoma, head and neck cancer, breast cancer) or in locations where heat monitoring is easier (eg, cervical and rectal cancers, sarcoma).[3] The recognition that urothelial carcinomas demonstrate improved chemosensitivity when heated makes the use of hyperthermia to treat bladder cancer quite appealing.
Effects of Hyperthermia on the Cancer Cell
TABLE
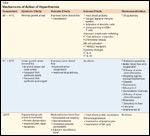
Mechanisms of Action of HyperthermiaFIGURE
Hyperthermia-induced Cell Death is Time and Temperature Dependent
The effect of hyperthermia on tumor cells is known to be multifactorial in nature (Table 1). Direct cell kill can occur with temperatures above 40.5°C, but this represents only a part of the benefit. Hyperthermia also cooperates with the myriad cellular, molecular, and metabolic derangements that occur just outside the direct heat kill zone to promote tumor necrosis and apoptosis. Supplemented by multimodal therapies such as chemotherapy or radiotherapy, a synergistic relationship, termed thermosensitization, can be created.
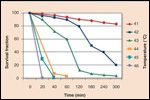
There are two phases of direct cytotoxicty associated with heat exposure.[4] The first phase is one of linear metabolic arrest that represents a period of reversible injury. The second phase is irreversible cytotoxicity and is easier to achieve with increasing temperatures; this more pronounced cytotoxicity is also related to the duration of exposure (Figure). There is a clear dose-response relationship between temperature and cell death, and the transition from the linear to the exponential phase of cytotoxicity occurs more easily at temperatures above 43°C. Although the requisite thermal dose for exponential cell death varies among tumor types, the experimental threshold required for protein denaturation and cell membrane disruption occurs at a dose of 140 kcal/mol.[5,6]
Supplementing this direct cytotoxicity is the observation that nuclear fragility is greatest during the S and M phases of cell life. The G1 and G2 phases are more resistant to cell death, a phenomenon that is thought to be due in part to the expression of adaptive heat-shock proteins.[7] The disruption of cellular transmembrane proteins involved in homeostatic ionic transport combines with architectural damage to ultimately yield cellular blebbing, which is characteristic of apoptosis. In addition, RNA synthesis and DNA synthesis are diminished at temperatures above 42°C. Although RNA synthesis recovers quickly after termination of heat exposure, DNA synthesis remains inhibited for a longer period due to the heat-induced unfolding of hydrophobic segments of protein, rendering them insoluble.[4]
Hyperthermia also has numerous effects on the vascular supply to the tumor. Acidosis leading to intravascular thrombosis, direct corpuscular injury, and the differential response of tumor endothelium are thought to be possible mechanisms of heat-related vascular injury.[8] Postulating that normal cells retain a superior ability to thermoregulate, Manfred von Ardenne proposed that whole-body hyperthermia (WBH) would create a peripheral hyperemia that, when combined with peripheral vasodilatory agents, could create an adjacent tissue vascular steal effect that would result in normal tissues outcompeting tumoral tissues for blood flow, resulting in intratumoral lactic acidosis and enhanced cytotoxicity.[9]
While the study of the tumor microenvironment demonstrates multifactorial vascular injury at temperatures above 43°C, maintaining such temperatures in vivo has proven much more difficult. Several other physiologic processes that are activated at sub-lethal temperatures have subsequently been uncovered; these help explain the clinical benefits of hyperthermia that are observed in the sublethal 41°-43°C range. One of these possible explanations is that the effects of heat can accumulate (ie, a cumulative thermal isoeffect dose effect) and induce cellular mechanisms of cell cycle arrest and apoptosis. Additionally, moderate hyperthermia actually increases tumor blood flow, thereby rendering the cells more susceptible to chemotherapy or radiation therapy.[10]
One mechanism by which the cell attempts to protect itself is thought to be the heat-induced expression of heat shock proteins (HSPs). These are a heterogeneous group of proteins that range in size from 40 to 100 kDa and that are expressed quickly through activation of response elements triggered by heat and other cellular stressors. HSPs are molecular chaperones, whose key duties are to protect cellular proteins from harm, to assist in their proper folding, and to shuttle them to appropriate locations in the cell (such as to sites of degradation). They do this by indiscriminately binding to hydrophobic segments of protein exposed as a result of denaturation; this prevents irreversible interactions between denatured proteins from occurring. HSPs thus protect the cell from heat and contribute to thermotolerance. Although HSP synthesis is induced by moderate degrees of hyperthermia, the production of HSPs is inhibited at higher temperatures; the exact temperature at which inhibition occurs is dependent on the cell type.[11]
Effects of Hyperthermia on the Immune System
It has been known for decades that hyperthermia has several important effects on the functioning of the immune system (Table).[12-14] Indeed, fever-range hyperthermia (39°-41°C) is thought to represent an evolutionary adaptation that has helped humans combat a wide range of infectious and immunologic attacks.[15] One of the principal mediators of the immune effects seen with hyperthermia is the HSP family mentioned above. Because HSPs are molecular chaperones, in a cancer-bearing patient they are expected at any given time to contain a sampling of the intracellular proteins currently being transcribed by cancer cells. HSPs are released from dying cancer cells that have been treated with heat in combination with chemotherapy and/or radiotherapy. These HSPs contain tumor-related antigens, abnormal proteins that are produced by cancer cells and recognized as foreign material by the immune system. Dendritic cells and other antigen-presenting cells exposed to the HSPs are not only exposed to the tumor antigens carried by the HSPs but they are also activated-since HSPs are interpreted as a danger signal.[16] The activation of dendritic cells with HSP-derived tumor antigens allows for the cross-priming activation of CD8+ cytotoxic T cells against these antigens, thereby triggering an acquired anti-tumor immune reponse.[17] Hyperthermia thus serves as a method of HSP-mediated auto-vaccination against the tumor.
In addition to improving the presentation of tumor antigen to T cells, hyperthermia also enhances leukocyte trafficking; this is an important effect, since lymphocytes must not only be activated against an antigen but must also be able to make their way to the tumor in order to attack it. Heat improves leukocyte trafficking by increasing Inter-Cellular Adhesion Molecule 1 (ICAM-1) expression on lymphoid high-endothelial venules and by enhancing the expression of L-selectin on lymphocytes.[18,19] This combination of influences allows T cells to stick to the lymphatic endothelium and migrate selectively into peripheral lymph nodes, thereby resulting in the accumulation of tumor-recognizing T cells at a site where they can have useful anti-tumor effects.[20,21] Hyperthermia also increases chemokine release in the vicinity of the tumor, enabling lymphocytes to selectively home to the appropriate site of action.[22,23]
Lastly, hyperthermia also activates the innate immune system. Natural killer (NK) cells in particular are a cell type that has been shown to be strongly influenced by hyperthermia.[24,25] Heat leads to clustering of antigen receptors (NKG2D) on the surface of the NK cell and to the expression of MICA on tumor cells, both of which lead to NK targeting of tumor cells.[26] In summary, heat activates both the acquired and innate branches of the immune system.
Hyperthermia as an Adjuvant to Radiation and Chemotherapy
Although cells in S phase have been observed to show a response to hyperthermia, cells in this phase are less susceptible to the effects of radiotherapy. However, a synergistic effect is noted when heat is combined with radiotherapy and thermal radiosensitization in cancer cells increases, a phenomenon that is especially apparent in cells in S phase.[27] It has been shown in vitro that heat obstructs the repair mechanism for radiation-damaged DNA via inhibition of DNA-polymerases α and β. The sequence of treatments is also quite important, with heat preceding radiation producing the greatest therapeutic ratio.[4]
Hyperthermia has also been noted to enhance the cytotoxicity of several chemotherapeutic agents.[28,29] The drug-heat interaction is best illustrated by a thermal enhancement ratio (TER). The TER as it relates to thermal chemosensitization is the ratio of cells that survive at a given temperature to those that survive at 37°C per chemotherapeutic agent used. Several ways of characterizing the drug-heat interaction have developed; these include “additive,” “threshold-activity,” and “independent.” Most alkylating agents (eg, cyclophosphamide, ifosfamide) and DNA cross-linking agents (eg, mitomycin C [MMC]) are observed to be more cytotoxic when combined with heat (“additive” drug-heat interaction).[30,31] DNA intercalators (eg, doxorubicin) demonstrate threshold-like behavior: little to no additional cytotoxicity is noted below a certain temperature, but beyond a threshold temperature an additive effect is observed.[32] For the most part, antimetabolites (eg, fluorouracil) demonstrate no improved effect when combined with hyperthermia and thus are characterized as “independent”.[33] The temporal relationship between the administration of hyperthermia and chemotherapy varies according to the drug given. With some drugs (eg, cyclophosphamide and gemcitabine [Gemzar]), maximal cytotoxicity is observed when they are given prior to hyperthermia, while others (eg, etoposide) work best when given during heat application.[34] One might assume that the hyperemia associated with hyperthermia would enhance drug delivery to tumor cells, but the pharmacokinetics and fidelity of the drugs themselves may also be affected. As the delivery mechanisms of hyperthermia advance, so will the study of thermal pharmacodynamics.
Thermal Dosimetry
Thermal dosimetry (thermometry) is critical to the optimization of hyperthermia treatment as well as to the minimization of potential heat-related toxicity. Although delivery standardization is difficult to implement because of varying target locations and clinical circumstances, Oleson and colleagues created the concept of the “thermal isoeffect dose,” which is used to quantitate a given thermal dose as “equivalent heating minutes” at 43°C.[35,36] Each additional 1°C doubles the equivalent number of minutes at 43°C. Each 1°C below 43°C effectively decreases the 43°C-equivalent time-dose by a factor of 4.[37] Tissue temperature has typically been recorded via invasive intratumoral thermistors or by a catheter placed in a hollow viscus (eg, the urethra, bladder, or rectum).[38,39]
Although dosimetry has advantages with regard to the evaluation of treatment temperature and the ability to modify the therapy dose as needed, the possible effects of thermal shielding, direct complications from probe placement, and patient discomfort must also be considered. Thus, other experimental models of thermal dosimetry measurement have been proposed. Recent investigation into the use of magnetic resonance (MR) imaging–based thermometry has proved very promising.[40] MR–temperature distribution mapping is a combined measurement of perfusion and tissue temperature.[41] Intratumoral perfusion can also be affected by hyperthermia, and this, too, can be imaged with MR.[42,43] Additionally, consideration has been given to the use of imaging-based thermometry techniques in conjunction with contrast-containing liposomes for hyperthermia-mediated drug delivery.[44]
Hyperthermia as a Treatment for Bladder Cancer
Although the concept of hyperthermia to treat malignancy has existed for many years, efforts to further its use had waned because of the technical limitations of tissue delivery. However, there has been renewed interest of late in the realm of urologic tumors, especially with regard to using hyperthermia to treat prostate and urothelial carcinomas. Urothelial carcinoma (UC) of the bladder is the fourth most common solid tumor in American men; although it has a widely variable pathologic presentation, 75% of patients present with non–muscle-invasive bladder cancer (NMIBC). The biology of UC is just as varied, with high-grade NMIBC progressing to invasive disease in a substantial number of cases.
Intravesical bacillus Calmette-Gurin (BCG) immunotherapy is commonly used as a first-line therapy to help prevent the progression of NMIBC to a muscle-invasive phenotype. When BCG therapy fails, it is a common practice for patients to consider radical cystectomy, an aggressive extirpative surgery associated with many side effects. In an effort to reduce the number of patients having to suffer the morbidity of radical cystectomy, alternative therapies are actively being sought. Additionally, many patients with low-grade NMIBC have recurrent tumors that may not be a threat to their life but that certainly can dramatically impair their quality of life. Patients with multi-recurrent disease are typically treated with intravesical BCG therapy, although other intravesical chemotherapies are also used. When these treatments fail and the tumors continue to recur, having alternative therapies available would be beneficial.
The additive effect of combining hyperthermia with chemotherapy has been validated in vitro several times.[32,45] For example, van der Heijden and colleagues demonstrated that MMC combined with hyperthermia induced incremental cytotoxicity in multiple human bladder cancer cell lines.[46] The following year, the same group from the Netherlands compared the effect of several chemotherapy agents used in combination with heat. Synergism was demonstrated with MMC and with epirubicin, and to a lesser extent with gemcitabine.[47] Animal studies have confirmed these data.[48]
These preclinical studies have led to human trials, and many patients with bladder cancer have been treated with hyperthermia, usually in combination with intravesical therapy. The most commonly used regimen is hyperthermia combined with 40 mg of intravesical MMC. Several studies using this approach have been published, although many of these studies unfortunately involve the same core group of investigators.[46,49-60]
Several conclusions can be derived from these studies. First, hyperthermia increases the absorption of MMC (although not to a level associated with myelosuppression), indicating that heat improves the penetrance of MMC across the bladder wall.[54] This effect suggests that heat helps deliver more MMC to the tumor, especially tumor hiding deeper in the bladder where it may be on the verge of progressing to muscle invasion.
Second, while hyperthermia does modestly increase treatment toxicity, it does not result in life-threatening events or the inability to complete therapy.[46,55,61] In fact, virtually all of the side effects of combination MMC and hyperthermia are mild and temporary and require minimal, if any, treatment.
Third, combination hyperthermia and MMC is better than MMC alone at preventing recurrences of NMIBC. This was best demonstrated in a randomized trial in which the NMIBC recurrence rate was 4.8 times higher in the MMC arm than in the MMC plus heat arm.[55] An earlier randomized trial showed similar results,[51] and together these studies demonstrate that MMC administered with heat is superior to MMC alone for preventing NMIBC recurrences.
Reference Guide
Therapeutic Agents
Mentioned in This Article
Bacillus Calmette-Gurin
Cyclophosphamide
Doxorubicin
Epirubicin
Etoposide
Fluorouracil
Gemcitabine (Gemzar)
Ifosfamide
Mitomycin C
Brand names are listed in parentheses only if a drug is not available generically and is marketed as no more than two trademarked or registered products. More familiar alternative generic designations may also be included parenthetically.
Fourth, when compared to historical controls treated with MMC alone, combination MMC and hyperthermia appears to reduce the risk of progression of NMIBC to muscle-invasive disease.[59] This conclusion is based on a progression rate of approximately 8% in patients treated with hyperthermia and MMC, compared with a historical rate of about 15% to 20% for MMC alone[62,63]-although the underlying progression risk in these populations may not be the same, making it difficult to draw firm conclusions.
Fifth, while patients in whom BCG immunotherapy has previously failed are generally considered to be at high risk for treatment failure, combination MMC and hyperthermia probably salvages more of these patients than MMC alone.[55,61] Sixth, the clinical response to combination MMC and hyperthermia can be long-lasting, with many patients (40% to 50%) remaining disease free at 3 to 5 years post-treatment.[59-61] Lastly, although the data in bladder cancer patients are sparse and definitive conclusions are difficult to draw, hyperthermia may also be combined with systemic chemotherapy and/or radiation therapy in patients with muscle-invasive bladder cancer, with the potential effect of improving treatment efficacy and/or providing a bladder-sparing result.[64,65] This type of strategy has been shown to be effective in other tumors, such as sarcoma,[66] cervical cancer,[67] breast cancer,[68] and rectal cancer.[65]
Conclusion
Modern technologies have changed our ability to accurately deliver and measure the dose of deep pelvic hyperthermia and have consequently sparked a renewed interest in using this therapeutic modality to treat bladder cancer. Trials are ongoing at our institution and others to further delineate who benefits from hyperthermia and how its delivery can be optimized.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
References
1. Barth G, Huth E, Wachsmann F. [Experimental investigations on hyperthermia therapy of neoplasms.]. Strahlentherapie. 1952;88:1-7.
2. Selawry OS, Goldstein MN, Mc CT. Hyperthermia in tissue-cultured cells of malignant origin. Cancer Res. 1957;17:785-91.
3. Wust P, Hildebrandt B, Sreenivasa G, et al. Hyperthermia in combined treatment of cancer. Lancet Oncol. 2002;3:487-97.
4. Hildebrandt B, Wust P, Ahlers O, et al. The cellular and molecular basis of hyperthermia. Crit Rev Oncol Hematol. 2002;43:33-56.
5. Dewey WC, Westra A, Miller HH, Nagasawa H. Heat-induced lethality and chromosomal damage in synchronized Chinese hamster cells treated with 5-bromodeoxyuridine. Int J Radiat Biol Relat Stud Phys Chem Med. 1971;20:505-20.
6. Westra A, Dewey WC. Variation in sensitivity to heat shock during the cell-cycle of Chinese hamster cells in vitro. Int J Radiat Biol Relat Stud Phys Chem Med. 1971;19:467-77.
7. Coss RA, Dewey WC, Bamburg JR. Effects of hyperthermia on dividing Chinese hamster ovary cells and on microtubules in vitro. Cancer Res. 1982;42:1059-71.
8. Vaupel P, Kallinowski F, Kluge M. Pathophysiology of tumors in hyperthermia. Recent Results Cancer Res. 1988;107:65-75.
9. Ardenne MV. [Synergic therapeutic effect of selective local hyperthermia and selective optimized hyperacidity against tumors. Theoretical and experimental bases]. Ther Ggw. 1977;116:1299-316.
10. Iwata K, Shakil A, Hur WJ, et al. Tumour pO2 can be increased markedly by mild hyperthermia. Br J Cancer Suppl. 1996;27:S217-21.
11. Jaattela M. Heat shock proteins as cellular lifeguards. Ann Med. 1999;31:261-71.
12. Vaughn LK, Bernheim HA, Kluger MJ. Fever in the lizard Dipsosaurus dorsalis. Nature. 1974;252:473-4.
13. Kluger MJ, Ringler DH, Anver MR. Fever and survival. Science. 1975;188:166-8.
14. Kluger MJ, Rothenburg BA. Fever and reduced iron: their interaction as a host defense response to bacterial infection. Science. 1979;203:374-6.
15. Kluger MJ. The evolution and adaptive value of fever. Am Sci. 1978;66:38-43.
16. Srivastava P. Interaction of heat shock proteins with peptides and antigen presenting cells: chaperoning of the innate and adaptive immune responses. Annu Rev Immunol. 2002;20:395-425.
17. Binder RJ, Srivastava PK. Peptides chaperoned by heat-shock proteins are a necessary and sufficient source of antigen in the cross-priming of CD8+ T cells. Nat Immunol. 2005;6:593-9.
18. Appenheimer MM, Chen Q, Girard RA, et al. Impact of fever-range thermal stress on lymphocyte-endothelial adhesion and lymphocyte trafficking. Immunol Invest. 2005;34:295-323.
19. Chen Q, Fisher DT, Clancy KA, et al. Fever-range thermal stress promotes lymphocyte trafficking across high endothelial venules via an interleukin 6 trans-signaling mechanism. Nat Immunol. 2006;7:1299-308.
20. Chen Q, Fisher DT, Kucinska SA, et al. Dynamic control of lymphocyte trafficking by fever-range thermal stress. Cancer Immunol Immunother. 2006;55:299-311.
21. Chen Q, Wang WC, Bruce R, et al. Central role of IL-6 receptor signal-transducing chain gp130 in activation of L-selectin adhesion by fever-range thermal stress. Immunity. 2004;20:59-70.
22. Robins HI, Kutz M, Wiedemann GJ, et al. Cytokine induction by 41.8 degrees C whole body hyperthermia. Cancer Lett. 1995;97:195-201.
23. Shah A, Unger E, Bain MD, et al. Cytokine and adhesion molecule expression in primary human endothelial cells stimulated with fever-range hyperthermia. Int J Hyperthermia. 2002;18:534-51.
24. Zanker KS, Lange J. Whole body hyperthermia and natural killer cell activity. Lancet. 1982;1:1079-80.
25. Dayanc BE, Beachy SH, Ostberg JR, Repasky EA. Dissecting the role of hyperthermia in natural killer cell mediated anti-tumor responses. Int J Hyperthermia. 2008;24:41-56.
26. Ostberg JR, Dayanc BE, Yuan M, et al. Enhancement of natural killer (NK) cell cytotoxicity by fever-range thermal stress is dependent on NKG2D function and is associated with plasma membrane NKG2D clustering and increased expression of MICA on target cells. J Leukoc Biol. 2007;82:1322-31.
27. Dewey WC, Thrall DE, Gillette EL. Hyperthermia and radiation--a selective thermal effect on chronically hypoxic tumor cells in vivo. Int J Radiat Oncol Biol Phys. 1977;2:99-103.
28. Issels RD. Hyperthermia and thermochemotherapy. Cancer Treat Res. 1993;67:143-60.
29. Issels RD. Hyperthermia adds to chemotherapy. Eur J Cancer. 2008;44:2546-54.
30. van der Heijden AG, Jansen CF, Verhaegh G, et al. The effect of hyperthermia on mitomycin-C induced cytotoxicity in four human bladder cancer cell lines. Eur Urol. 2004;46:670-4.
31. Longo FW, Tomashefsky P, Rivin BD, Tannenbaum M. Interaction of ultrasonic hyperthermia with two alkylating agents in a murine bladder tumor. Cancer Res. 1983;43:3231-5.
32. Uchibayashi T, Lee SW, Kunimi K, et al. Studies of effects of anticancer agents in combination with/without hyperthermia on metastasized human bladder cancer cells in chick embryos using the polymerase chain reaction technique. Cancer Chemother Pharmacol. 1994;35 Suppl:S84-7.
33. Dahl O. Interaction of hyperthermia and chemotherapy. Recent Results Cancer Res. 1988;107:157-69.
34. Wiedemann GJ, Siemens HJ, Mentzel M, et al. Effects of temperature on the therapeutic efficacy and pharmacokinetics of ifosfamide. Cancer Res. 1993;53:4268-72.
35. Oleson JR, Samulski TV, Leopold KA, et al. Sensitivity of hyperthermia trial outcomes to temperature and time: implications for thermal goals of treatment. Int J Radiat Oncol Biol Phys. 1993;25:289-97.
36. Sapareto SA. Thermal isoeffect dose: addressing the problem of thermotolerance. Int J Hyperthermia. 1987;3:297-305.
37. Wust P, Cho CH, Hildebrandt B, Gellermann J. Thermal monitoring: invasive, minimal-invasive and non-invasive approaches. Int J Hyperthermia. 2006;22:255-62.
38. Fatehi D, Van Der Zee J, Wielheesen DH, et al. Intra-luminal thermometry: is tissue type assignment a necessity for thermal analysis? Int J Hyperthermia. 2006;22:463-73.
39. Wust P, Gellermann J, Harder C, et al. Rationale for using invasive thermometry for regional hyperthermia of pelvic tumors. Int J Radiat Oncol Biol Phys. 1998;41:1129-37.
40. Gellermann J, Wlodarczyk W, Hildebrandt B, et al. Noninvasive magnetic resonance thermography of recurrent rectal carcinoma in a 1.5 Tesla hybrid system. Cancer Res. 2005;65:5872-80.
41. Gellermann J, Hildebrandt B, Issels R, et al. Noninvasive magnetic resonance thermography of soft tissue sarcomas during regional hyperthermia: correlation with response and direct thermometry. Cancer. 2006;107:1373-82.
42. Gellermann J, Wlodarczyk W, Feussner A, et al. Methods and potentials of magnetic resonance imaging for monitoring radiofrequency hyperthermia in a hybrid system. Int J Hyperthermia. 2005;21:497-513.
43. Peller M, Kurze V, Loeffler R, et al. Hyperthermia induces T1 relaxation and blood flow changes in tumors. A MRI thermometry study in vivo. Magn Reson Imaging. 2003;21:545-51.
44. Tashjian JA, Dewhirst MW, Needham D, Viglianti BL. Rationale for and measurement of liposomal drug delivery with hyperthermia using non-invasive imaging techniques. Int J Hyperthermia. 2008;24:79-90.
45. Nakajima K, Hisazumi H. Enhanced radioinduced cytotoxicity of cultured human bladder cancer cells using 43 degrees C hyperthermia or anticancer drugs. Urol Res. 1987;15:255-60.
46. van der Heijden AG, Kiemeney LA, Gofrit ON, et al. Preliminary European results of local microwave hyperthermia and chemotherapy treatment in intermediate or high risk superficial transitional cell carcinoma of the bladder. Eur Urol. 2004;46:65-71; discussion -2.
47. van der Heijden AG, Verhaegh G, Jansen CF, et al. Effect of hyperthermia on the cytotoxicity of 4 chemotherapeutic agents currently used for the treatment of transitional cell carcinoma of the bladder: an in vitro study. J Urol. 2005;173:1375-80.
48. Rath-Wolfson L, Moskovitz B, Dekel Y, et al. Combined intravesical hyperthermia and mitomycin chemotherapy: a preliminary in vivo study. Int J Exp Pathol. 2003;84:145-52.
49. Rigatti P, Lev A, Colombo R. Combined intravesical chemotherapy with mitomycin C and local bladder microwave-induced hyperthermia as a preoperative therapy for superficial bladder tumors. A preliminary clinical study. Eur Urol. 1991;20:204-10.
50. Colombo R, Lev A, Da Pozzo LF, et al. A new approach using local combined microwave hyperthermia and chemotherapy in superficial transitional bladder carcinoma treatment. J Urol. 1995;153:959-63.
51. Colombo R, Da Pozzo LF, Lev A, et al. Neoadjuvant combined microwave induced local hyperthermia and topical chemotherapy versus chemotherapy alone for superficial bladder cancer. J Urol. 1996;155:1227-32.
52. Colombo R, Da Pozzo LF, Lev A, et al. Local microwave hyperthermia and intravesical chemotherapy as bladder sparing treatment for select multifocal and unresectable superficial bladder tumors. J Urol. 1998;159:783-7.
53. Colombo R, Brausi M, Da Pozzo L, et al. Thermo-chemotherapy and electromotive drug administration of mitomycin C in superficial bladder cancer eradication. a pilot study on marker lesion. Eur Urol. 2001;39:95-100.
54. Paroni R, Salonia A, Lev A, et al. Effect of local hyperthermia of the bladder on mitomycin C pharmacokinetics during intravesical chemotherapy for the treatment of superficial transitional cell carcinoma. Br J Clin Pharmacol. 2001;52:273-8.
55. Colombo R, Da Pozzo LF, Salonia A, et al. Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma. J Clin Oncol. 2003;21:4270-6.
56. Gofrit ON, Shapiro A, Pode D, et al. Combined local bladder hyperthermia and intravesical chemotherapy for the treatment of high-grade superficial bladder cancer. Urology. 2004;63:466-71.
57. Moskovitz B, Meyer G, Kravtzov A, et al. Thermo-chemotherapy for intermediate or high-risk recurrent superficial bladder cancer patients. Ann Oncol. 2005;16:585-9.
58. Alfred Witjes J, Hendricksen K, Gofrit O, et al. Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo working party. World J Urol. 2009;27:319-24.
59. Halachmi S, Moskovitz B, Maffezzini M, et al. Intravesical mitomycin C combined with hyperthermia for patients with T1G3 transitional cell carcinoma of the bladder. Urol Oncol. 2009.
60. Nativ O, Witjes JA, Hendricksen K, et al. Combined thermo-chemotherapy for recurrent bladder cancer after bacillus Calmette-Guerin. J Urol. 2009;182:1313-7.
61. Witjes JA, Hendricksen K, Gofrit O, et al. Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo working party. World J Urol. 2009;27:319-24.
62. Malmstrom PU, Sylvester RJ, Crawford DE, et al. An individual patient data meta-analysis of the long-term outcome of randomised studies comparing intravesical mitomycin C versus bacillus Calmette-Guerin for non-muscle-invasive bladder cancer. Eur Urol. 2009;56:247-56.
63. Sylvester RJ, van der Meijden AP, Witjes JA, Kurth K. Bacillus Calmette-Guerin versus chemotherapy for the intravesical treatment of patients with carcinoma in situ of the bladder: a meta-analysis of the published results of randomized clinical trials. J Urol. 2005;174:86-91; discussion -2.
64. Bichler KH, Fluchter SH, Steimann J, Strohmaier WL. Combination of hyperthermia and cytostatics in the treatment of bladder cancer. Urol Int. 1989;44:10-4.
65. van der Zee J, Gonzalez Gonzalez D, van Rhoon GC, et al. Comparison of radiotherapy alone with radiotherapy plus hyperthermia in locally advanced pelvic tumours: a prospective, randomised, multicentre trial. Dutch Deep Hyperthermia Group. Lancet. 2000;355:1119-25.
66. Issels RD, Lindner LH, Verweij J, et al. Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft-tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol. 2010;11:561-70.
67. Franckena M, Stalpers LJ, Koper PC, et al. Long-term improvement in treatment outcome after radiotherapy and hyperthermia in locoregionally advanced cervix cancer: an update of the Dutch Deep Hyperthermia Trial. Int J Radiat Oncol Biol Phys. 2008;70:1176-82.
68. Jones EL, Oleson JR, Prosnitz LR, et al. Randomized trial of hyperthermia and radiation for superficial tumors. J Clin Oncol. 2005;23:3079-85.