Lymphadenectomy Indicated in Stage IA Ovarian Cancer
NEW ORLEANS-With few exceptions, lymphadenectomy should be performed in ovarian cancer patients even if they have stage IA disease. This was the conclusion of French investigators who analyzed 276 women with epithelial ovarian cancer and reported their results at the 34th Annual Meeting of the Society of Gynecologic Oncologists (abstract 94).
NEW ORLEANSWith few exceptions, lymphadenectomy should be performed in ovarian cancer patients even if they have stage IA disease. This was the conclusion of French investigators who analyzed 276 women with epithelial ovarian cancer and reported their results at the 34th Annual Meeting of the Society of Gynecologic Oncologists (abstract 94).
The study aimed to determine the factors that influence nodal involvement and the topography of the pelvic and para-aortic nodal involvement in ovarian cancer. The goal was to deduce surgical implications, particularly in patients with apparent early-stage disease.
"In other words, we asked whether removal of the lymph nodes always adds therapeutic value, whether there is a need for lymphadenectomy in all patients," said lead investigator Philippe Morice, MD, of the Institute Gustave-Roussy, Villejuif, France.
The conclusion of the study was that bilateral lymph node dissection should be performed, even in cases of patients with unilateral tumors. The exception would be in patients with mucinous apparent stage I disease and stage I grade 1 tumors. In these patients, nodal involvement was not seen in this series.
The study was a review of 276 women who underwent a systematic bilateral pelvic and para-aortic lymphadenectomy between 1985 and 2001. Preoperative chemotherapy was given to 105 patients while 171 received no preoperative chemotherapy. The procedure generally was a complete bilateral resection by laparotomy to the level of the left renal vein. A median of 14 pelvic and 15 para-aortic nodes were removed.
Complications included lymphocysts in 13.8%, major vascular injuries in 0.5%, and damage to ureters or development of fistulae in 1.8%.
Findings in Lymph Nodes
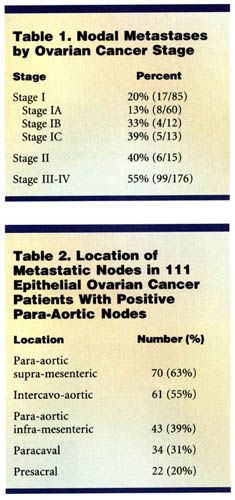
Of the 276 patients in the study, 122 (44%) had positive lymph nodes. The frequencies of pelvic and para-aortic metastases were 30% (82 patients) and 40% (111 patients), respectively. The frequency of lymph node metastases according to the stage of disease is shown in Table 1 below. Table 2 shows the location of metastatic nodes in the patients with positive para-aortic nodes.
None of the patients with stage I grade 1 disease had nodal involvement, nor did any of the patients with mucinous tumor confined to the ovaries, Dr. Morice reported.
Histologic subtypes included serous in over half of the patients, followed by endometroid and mucinous.
Preoperative chemotherapy did not appear to modify the rates of nodal spread. In patients who underwent preoperative chemotherapy, nodal involvement was seen in 14% of stage I patients, he said.
In patients with positive pelvic nodes, the external iliac nodes were involved in 79% of women and the obturator in 43%. When para-aortic nodes were involved, the most frequent site was the left para-aortic chain above the level of the inferior mesenteric artery (63% of patients). One of 9 patients (11%) with a macroscopic stage I unilateral tumor and para-aortic involvement had contralateral metastases.
"Our conclusion is that para-aortic nodes above the level of the inferior mesenteric artery are the most frequent site of positive nodes. There are contralateral positive lymph nodes in 11% of patients with early-stage disease, which indicates the need for a complete bilateral lymphadenectomy in all patients," Dr. Morice said. "We believe, however, that you can avoid this procedure in patients with stage I grade 1 disease and/or stage I mucinous tumors."
The discussant of the paper, Gregory P. Sutton, MD, of St. Vincent Hospitals and Health Services, Indianapolis, said that "in a perfect world, all epithelial ovarian cancer patients would have pelvic and para-aoric lymphadenectomy. Since there were only 20 patients with stage IA grade 1 tumors in this study, we cannot recommend ignoring nodes in this population. Patients with extensive stage IIIC and stage IV disease may not benefit from lymphadenectomy."