(S036) The Low Alpha-Beta Ratio of Bladder Cancer: A Rationale for Hypofractionation
We hypothesized that the promising outcomes with partial-bladder treatment might be due to the effects of hypofractionation. We thus aimed to analyze the clinical impact of hypofractionation on local control and to characterize the radiation response of a bladder cancer cell line with regard to clonogenic survival.
S036: Figures
Jung Julie Kang, MD, PhD, Keisuke S. Iwamoto, PhD, Elizabeth M. Peek, BS, Arnold I. Chin, MD, PhD, Christopher R. King, PhD, MD; Department of Radiation Oncology and Department of Urology and Molecular Biology Institute, University of California, Los Angeles
Purpose and Objectives: Surgery and chemoradiation are comparable treatments for muscle-invasive bladder cancer. A randomized trial in the UK recently showed equivalent outcomes with partial- and whole-bladder irradiation and even reported trends toward improved local control and survival with partial-bladder treatment. Partial-bladder radiation differs from whole-bladder treatment in three critical ways: the target volume is reduced, the treatment course is shortened, and the daily dose is typically hypofractionated.
We hypothesized that the promising outcomes with partial-bladder treatment might be due to the effects of hypofractionation. We thus aimed to analyze the clinical impact of hypofractionation on local control and to characterize the radiation response of a bladder cancer cell line with regard to clonogenic survival.
Materials and Methods: We retrospectively reviewed our institutional experience with clinical stage T2–4 N0–2 bladder cancer patients treated with definitive organ preservation chemoradiation from 2009–2012. Patients who were treated with a hypofractionated course (HF; 2.5 Gy/fx to a total tumor dose of 62.5 Gy, n = 16) were compared with conventionally fractionated patients (CF; 1.8 Gy/fx to a total tumor dose of 59.4–70.2 Gy, n = 7). All patients received pelvic nodal irradiation (45–50.4 Gy at 1.8–2 Gy/fx). Treatment was delivered via intensity-modulated radiation therapy with cone-beam CT image guidance (daily for HF). Concurrent radiosensitizing chemotherapy (typically platinum) was administered. Mean follow-up was 20 ± 3 months. Local control was defined as absence of progressive or recurrent disease within the bladder.
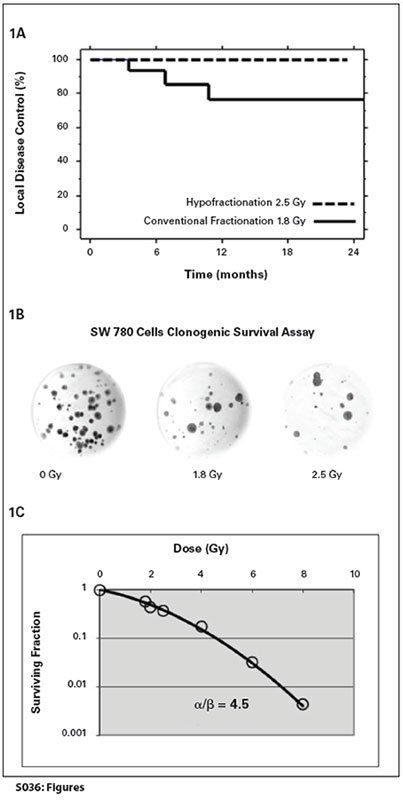
An immortalized human bladder cancer cell line, SW780 (ATCC), was used for in vitro studies. Clonogenic survival assay was performed on exponentially growing cells, which were trypsinized, counted, and diluted accordingly. Cell suspensions were irradiated at doses of 0, 1.8, 2, 2.5, 4, 6, and 8 Gy using a 137Cs laboratory irradiator at a dose rate of 4.21 Gy/min. Cells were then plated in 100-mm dishes in triplicate. After 21 days, colonies were fixed and stained with crystal violet in 70% ethanol. Colonies consisting of > 50 cells were counted to determine surviving fractions.
Results: No patients who received hypofractionated treatment had local failure in the bladder. There were only three LENT-SOMA late grade 3 ureteral toxicities (2 CF, 1 HF) and one acute grade 4 renal toxicity (CF), all of which resolved with management of ureteral obstruction. There appeared to be a difference in 2-year local control: 100% HF (7/7) vs 82% CF (13/16) [see Figure 1A]. The alpha-beta ratio was calculated to be 4.5 Gy for SW780 cells [Figures 1B, 1C].
Conclusions: Hypofractionated chemoradiation is an effective and well-tolerated treatment for bladder cancer. In fact, hypofractionation appears to provide better local disease control than conventional fractionation, although the study was underpowered to validate this observation. In vitro data suggest that bladder cancer cells have a lower alpha-beta ratio than most tumors, more closely approximating normal tissue values. The low alpha-beta ratio of bladder cancer may provide a radiobiological explanation for the efficacy of hypofractionation. Future studies of the effects of chemotherapy may provide valuable insight into enhancing the therapeutic ratio with radiosensitization as well as altered fractionation.
Proceedings of the 96th Annual Meeting of the American Radium Society - americanradiumsociety.org