(S005) Adjuvant Radiotherapy in Stage II Endometrial Carcinoma: Is Brachytherapy Alone Sufficient for Local Control?
To evaluate recurrence patterns and overall survival in patients treated with adjuvant radiation after surgical staging for stage II endometrial carcinoma. Secondary goals include identification of prognostic factors for recurrence.
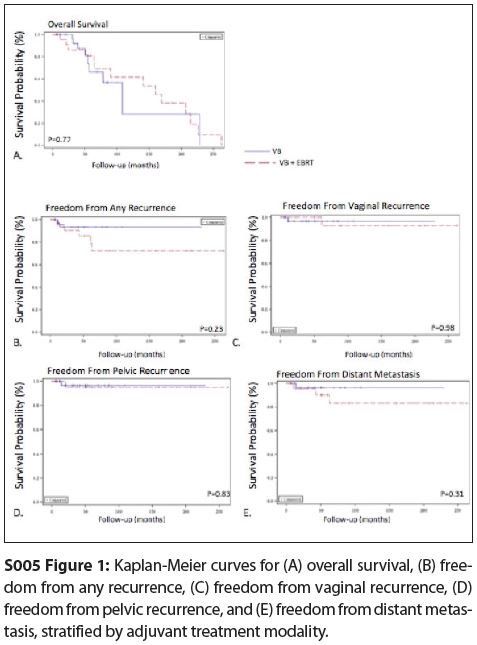
S005 Figure 1
Ima Paydar, MD, Todd DeWees, PhD, Matthew Powell, MD, David Mutch, MD, Perry W. Grigsby, MD, MS, Julie K. Schwarz, MD, PhD; Washington University School of Medicine
Objective: To evaluate recurrence patterns and overall survival in patients treated with adjuvant radiation after surgical staging for stage II endometrial carcinoma. Secondary goals include identification of prognostic factors for recurrence.
Materials and Methods: The medical records of 62 patients treated with adjuvant radiotherapy at Washington University School of Medicine following surgical staging for endometrial cancer (total abdominal hysterectomy and bilateral salpingo-oophorectomy, peritoneal cytology, and lymph node dissection) were reviewed. Twenty-six were treated with a combination of external beam radiotherapy and vaginal brachytherapy (EBRT + VB), and 36 patients were treated with postoperative vaginal brachytherapy (VB) alone. Median follow-up for all patients was 48 months.
Results: Median patient age was 61 years (range: 30–87 yr). All tumors had endometrioid histology. There were 30 grade 1 tumors, 20 grade 2 tumors, and 12 grade 3 tumors. For all patients, the 5-year overall survival was 75.4%, and the 5-year recurrence-free survival was 89%. There was no statistically significant difference in overall survival (P = .770) or freedom from vaginal (P = .981), pelvic (P = .834), distant (P = .307), or any recurrence (P = .230) with respect to modality of treatment (EBRT + VB vs VB alone) (Figure). In the multivariate analysis, the only risk factor influencing overall survival was patient age (P = .033). Four patients experienced a toxicity requiring hospital admission, and all of these patients were treated with pelvic external beam plus brachytherapy.
Conclusions: Vaginal brachytherapy alone results in excellent local control for patients with stage II endometrial cancer after surgical staging. Long-term toxicities are rare and are more common in patients who are treated with pelvic external beam plus brachytherapy.
Proceedings of the 96th Annual Meeting of the American Radium Society - americanradiumsociety.org