(S013) Adjuvant Radiation Therapy and Temozolomide for Anaplastic Gliomas: The Twelve-Year Washington University Experience
In this study, we present our institutional data on the clinical outcomes of radiation therapy plus temozolomide for anaplastic gliomas.
Table S013
Christina K. Speirs, MD, PhD, Joseph R. Simpson, MD, PhD, Clifford G. Robinson, MD, David D. Tran, MD, PhD, Gerry Linette, MD, Michael R. Chicoine, MD, Ralph G. Dacey, MD, Keith M. Rich, MD, Joshua L. Dowling, MD, Eric C. Leuthardt, MD, Gregory J. Zipfel, MD, Albert H. Kim, MD, PhD, Jiayi Huang, MD; Washington University School of Medicine
Background: Anaplastic gliomas represent a heterogeneous group of different pathological entities, and the optimal treatment approach after surgery remains controversial for different subtypes. Recently, long-term results of two randomized studies have shown that radiation therapy (RT) with procarbazine, lomustine, and vincristine (PCV) chemotherapy improved outcomes of those with codeletion of 1p/19q. Another combined modality approach, RT and temozolomide (TMZ), has also gained popularity in the treatment of anaplastic gliomas but has not been validated extensively. In this study, we present our institutional data on the clinical outcomes of RT + TMZ for anaplastic gliomas.
Methods: A single-institutional retrospective review was conducted on patients with intracranial anaplastic oligodendroglioma (AO), mixed anaplastic oligoastrocytoma (AOA), and anaplastic astrocytoma (AA) who were treated with adjuvant RT and TMZ after surgery. RT was delivered with either 3D conformal RT (3DCRT) or intensity-modulated RT (IMRT) to a median total dose of 60 Gy (range: 31.6–63 Gy) in daily fractions (median 2 Gy/fraction; range: 1.8–2.2 Gy/fraction). All patients received standard concurrent TMZ, with (90% of patients analyzed) or without maintenance TMZ (10%). Follow-up time was calculated from the start of RT.
Results: From 2000 to 2012, 111 cases met the study criteria and were evaluable: 20% AO, 33% AOA, and 47% AA. Median follow-up time was 2.43 years (range: 0.06–12.1 yr) but was 4.10 years (range: 0.8–12.1 yr) for living patients. All AOs and AOAs were evaluated for 1p/19q codeletions, and 42% had codeletions of 1p/19q. Pathology subtypes showed distinctively different outcomes. Non-codeleted AOs/AOAs displayed a trend of worse progression-free survival (PFS) than codeleted AOs/AOAs (46% vs 70% at 5 years, respectively; P = .10), while demonstrating significantly worse overall survival (OS) (68% vs 91% at 5 years, respectively; P = .02). Interestingly, AAs had significantly worse PFS and OS than noncodeleted AOs/AOAs (PFS: 27% vs 46% at 5 years, respectively; P = .03; OS: 37% vs 68% at 5 years, respectively; P = .007). Univariate analyses showed that age, Karnofsky performance score (KPS), surgical extent, pathology, and adjuvant TMZ were significant factors for PFS, while age, KPS, surgical extent, and pathology were significant factors for OS. On multivariate analysis, only age, KPS, and pathology (hazard ratio [HR] = 6.54 for OS in non-codeleted vs codeleted AOs/AOAs; HR = 15.6 for OS in AAs vs codeleted AOs/AOAs) were significant factors for both PFS and OS.
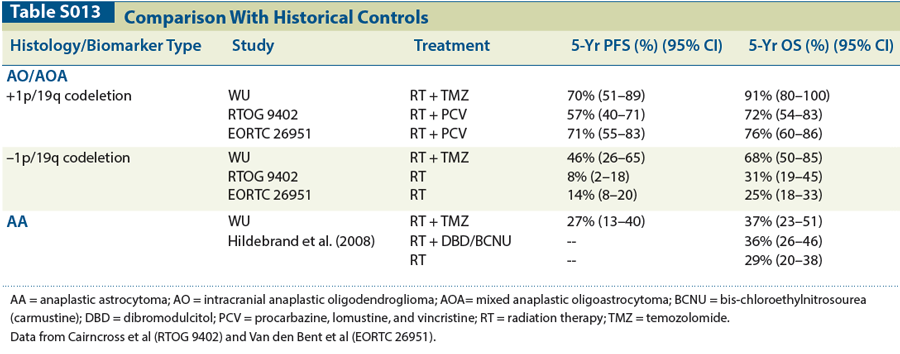
Conclusions: In patients treated with surgery followed by RT + TMZ, outcomes were dependent on pathology as follows: codeleted AO/AOA > non-codeleted AO/AOA > AA. As compared with historical controls from previous randomized studies (Table), codeleted AOs/AOAs treated with RT + TMZ achieved comparable results as those of RT + PCV, while non-codeleted AOs/AOAs that were treated with RT + TMZ appeared to have superior outcomes compared with RT alone. In contrast, AAs that were treated with RT + TMZ had similar results as those of RT alone. RT + TMZ may be a reasonable alternative approach for both codeleted and non-codeleted AOs/AOAs but may need further validation for AA patients.
Proceedings of the 96th Annual Meeting of the American Radium Society - americanradiumsociety.org