Superselective chemo strategies for HCC
Delivery of chemotherapy to hepatic artery branches that only or mainly feed a tumor—so-called superselective chemoembolization and chemoinfusion—yields favorable outcomes in patients with hepatocellular carcinoma (HCC)
SEATTLEDelivery of chemotherapy to hepatic artery branches that only or mainly feed a tumorso-called superselective chemoembolization and chemoinfusionyields favorable outcomes in patients with hepatocellular carcinoma (HCC), according to a pair of studies reported at the Society of Interventional Radiology annual meeting.
Daniel Yung-Ho Sze, MD, PhD, of Stanford University, explained the rationale for superselective chemoembolization: "We can give very high local doses of chemotherapy, prolong the dwell time of the chemotherapy, induce ischemia in the tumor, and limit the amount of organic as well as systemic toxicity of the chemotherapeutic agents."
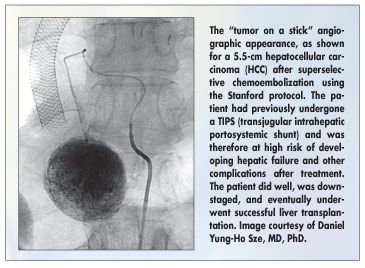
Dr. Sze cited two landmark randomized trials showing that chemoembolization reduces the risk of death by about half relative to supportive care in patients with HCC (Lancet 359:1734-1739, 2002, and Hepatology 35:1164-1171, 2002).The technical aspects of superselective chemoembolization are still debated, Dr. Sze noted. "Our protocol at Stanford is to maximize the superselectivity with microcatheters and minimize the amount of solid particulate embolization we use," he said. The Stanford protocol is derived from those widely used in Asia.Angiographically, this procedure produces a characteristic "tumor on a stick" appearance (see Figure).
In this retrospective study (abstract 153), the investigators assessed outcomes in 165 patients with HCC who underwent 345 superselective chemoembolization procedures, either to palliate symptoms or to maintain candidacy for transplantation. Dr. Sze recognized Dr. Bo Yoon Ha, of Seoul National Medical Center, and Dr. Mindie Nguyen, of Stanford, for compiling and analyzing the data.
Up to 20 mL of ethiodized oil (Ethio-dol), 50 mg cisplatin, and 50 mg doxorubicin were used. Particulate material, a slurry of absorbable gelatin sponge (Gelfoam), was added to treatment in only 12% of patients.
Chemoembolization Results
After censoring of patients who went on to liver transplant, 69%, 46%, 39%, and 30% of patients were alive at 1, 2, 3, and 4 years, respectively. "With multivariate analysis, all the things we thought were importanttotal bilirubin and albumin, prothrombin/INR, and plateletsreally didn't have much of an effect," he said.The only significant predictor of survival was TNM stage. The 3-year overall survival value (39%) was roughly similar to values obtained in the two landmark trials (26% to 29%), Dr. Sze commented.
After 99% of the superselective procedures, patients were discharged within 24 hours. The 30-day rate of treatment-related mortality was 0.3% of procedures and 0.6% of patients. Severe complications, excluding nausea, vomiting, or pain requiring prolongation of hospitalization, occurred in about 1% of procedures and 3% of patientsvalues that were lower by an order of magnitude than those of the previous two landmark trials (17% of procedures, 23% of patients).
"We all accept now that chemoembolization does
prolong life. The optimal technique though is still very controversial," Dr. Sze said. "We can say that superselectivity and gentle embolization (as performed in Asia) do seem to decrease the rates of adverse events and severe complications without substantially adversely affecting efficacy."
Young Ho So, MD, of Seoul National University Hospital, and his coinvestigators assessed the efficacy of superselective chemoinfusion when added to conventional transcatheter arterial chemoembolization (TACE) in 36 patients with advanced HCC with angioinvasion (abstract 151). The patients underwent TACE alone (n = 21) or TACE plus superselective chemoinfusion (n = 15).
TACE was performed with an emulsion of iodized oil and doxorubicin, and gelatin sponge particles. Superselective chemoinfusion included cisplatin (mean, 50 to 100 mg) infused as selectively as possible to tumor-feeding arteries using microcatheters, after TACE and, in patients without extrahepatic collaterals and with slow blood flow, also before TACE.
Chemoinfusion Results
Compared with TACE only, TACE plus superselective chemoinfusion produced higher 6-month rates of complete response (7% vs 0%), partial response, (47% vs 10%), and stable disease (27% vs 4%), and a lower rate of progressive disease (19% vs 86%). In a logistic regression analysis, treatment method was the only significant determinant factor for tumor response among the variables.
The pattern was similar when response of the hepatic vein and inferior vena cava invasion was assessed. Patients treated with TACE/chemoinfusion were more likely to have this invasion disappear (7% vs 0%), partially decrease (40% vs 0%), or remain stable (40% vs 29%), and were less likely to have it worsen (13% vs 71%).
Among the patients whose initial alfa-fetoprotein level was greater than 400 ng/mL, more patients in the combined treatment group had a fall in levels, and the magnitude of decrease was greater.
More patients in the TACE plus superselective chemoinfusion group had moderate-to-severe pain (87% vs 48%), nausea/vomiting (47% vs 19%), and fever (60% vs 38%). "But there were no major complications or hospitalization for more than 1 week," Dr. So noted.
Six-month overall survival was significantly better with TACE/chemoinfusion. Treatment method was the only significant prognostic factor for survival at 12 months. "Superselective hepatic artery chemoinfusion combined with conventional TACE improves early local control of the primary tumor and hepatic venous thrombosis in HCC without added risk of complications," Dr. So said.