A 65-Year-Old Man With Back Pain and Imaging Findings of Spinal Cord Compression
Mehmet S. Copur, MD, and colleagues examine the case of a 65-year-old who presented with back pain and a large T8 spinal mass, leading to a diagnosis of multiple myeloma with spinal cord compromise.
ABSTRACT: Spinal cord compression is a potentially devastating consequence of cancer. Early recognition of the signs and symptoms permit diagnosis prior to the development of irreversible neurological damage. This complication occurs in 5% to 10% of patients with malignancy, often at the end stages of the patient’s illness; however, it can be the presenting manifestation of malignancy in up to 23% of patients. With the advances in surgical, radiation, and medical oncology approaches, the outcomes of patients with malignant spinal cord compression continue to improve. We discuss the case of a previously healthy man, aged 65 years, who presented with back pain and a large T8 spinal mass, leading to a diagnosis of multiple myeloma with spinal cord compromise.
Oncology (Williston Park). 2021;35(3):128-133.
DOI: 10.46883/ONC.2021.3503.0128
Introduction
Spinal vertebral bone involvement with or without neurological deterioration can occur as a skeletal-related event in various cancers. The true incidence of malignant spinal cord compression is not known, but the estimate is about 15% in patients with advanced cancer.1 Metastases to the spine occur most commonly in patients with breast, prostate, and lung cancer, followed by those with renal, gastrointestinal, and thyroid cancer and malignant melanoma.2 Multiple myeloma is among the most common hematological malignancies leading to this complication. The spinal cord compression may present as a primary tumor (solitary plasmacytoma) or as part of the systemic involvement of multiple myeloma.3-5 Direct tumor extension into the vertebral column or the collapse of a vertebral body that contains metastatic disease can lead to the compression of the spinal cord. Initially, this causes reversible edema, venous congestion, and demyelination, followed by vascular injury and cord necrosis. With prolonged compression, permanent neurological damage occurs. Appropriate treatment of malignant spinal cord compression is complex and requires a multidisciplinary team approach.
Regardless of the tumor histology causing the spinal cord compression, the 3 most widely utilized treatment modalities have been surgery, radiation therapy (RT), and the administration of glucocorticoids, with or without systemic anticancer therapy. The introduction of new spinal instrumentations and surgical approaches, along with advances in radiation and medical oncology treatments, has considerably improved the extent of therapeutic options, resulting in better outcomes. Identifying the patients who would most benefit from what initial approach—surgical, radiation, or medical treatment—is the most crucial part of appropriate management.
Case
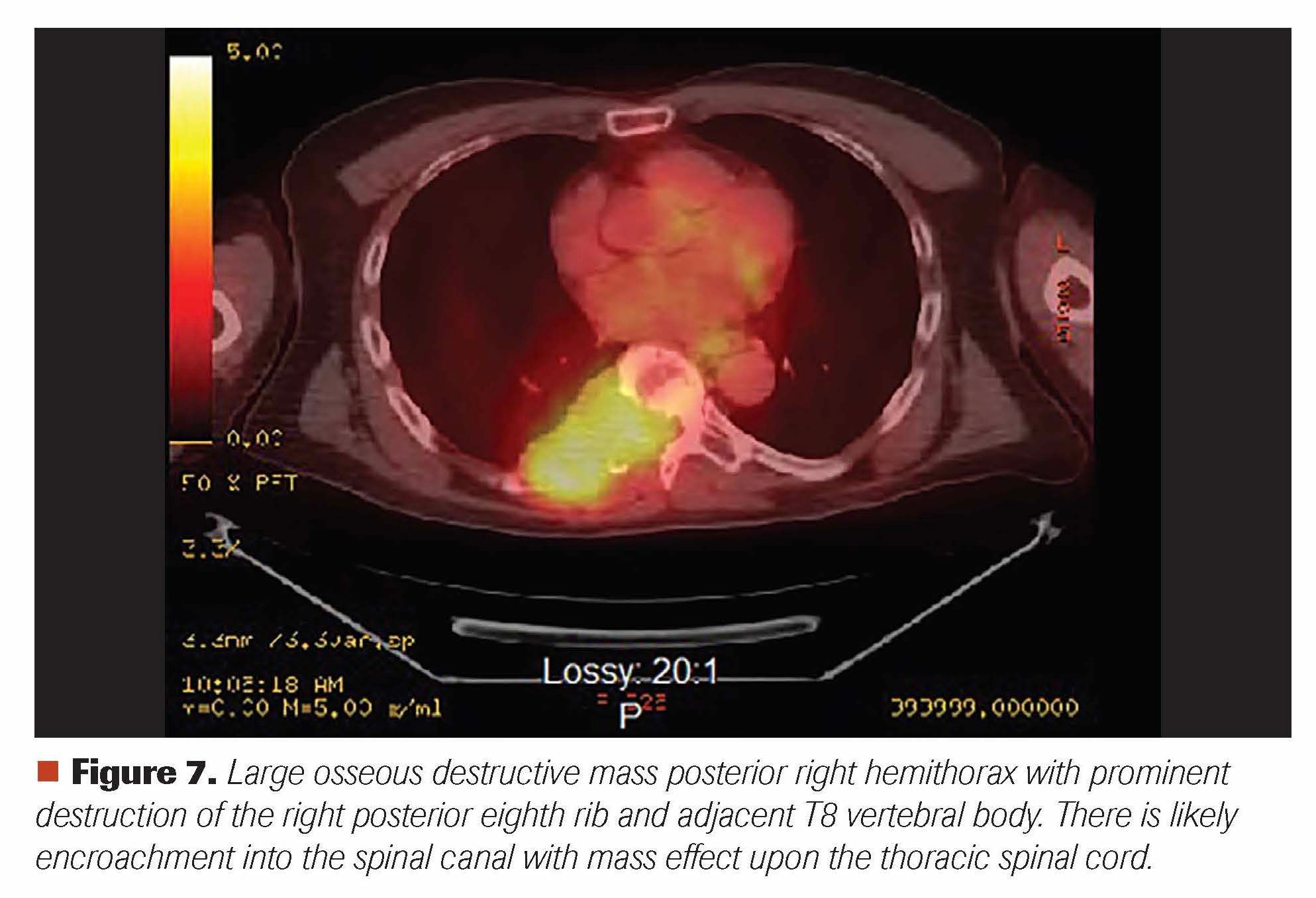
A man aged 65 years presented with right-sided lower thoracic back pain of 1-month duration; it was brought upon by pushing a sliding door in his garage. While it was initially a sharp pain, it transformed into a dull continuous ache radiating to his right rib and right hemithorax. He thought he pulled a muscle and saw a chiropractor, but he received no relief despite 5 chiropractic treatment sessions. During all this time he did not notice any extremity weakness or bladder or bowel incontinence, but he eighth area. He next saw his primary care provider, and a CT scan of his chest revealed a soft tissue mass measuring 6.2 x 3.5 x 2.8 cm in the posterior mediastinum/posterior chest wall with involvement of the posterior eighth rib and adjacent T8 vertebral body, with extension into the right aspect of the spinal canal (Figure 1). Further evaluation with an MRI of the thoracic spine confirmed the T8 compression and associated soft-tissue mass causing moderate-to-severe central spinal stenosis (Figure 2). A CT-guided biopsy of this large destructive mass revealed sheets of plasma cells (Figures 3 and 4). Further work-up revealed abnormal serum protein electrophoresis with a 3.53 g/dL monoclonal serum paraprotein, abnormal serum immunoglobulins (Ig; 5365 mg/dl; IgA, 23 mg/dL; IgM, 11 mg/dL), abnormal free light chains (λ free light chain, 14.6 mg/L; λ free light chain, 146.2 mg/L; ratio, 0.1), and abnormal λ-2 microglobulin of 4.9 mg/L. Bone marrow aspiration and biopsy revealed plasma cell myeloma comprising 40% of marrow cellularity (Figures 5 and 6). Staging work-up was completed with a PET-CT, confirming large osseous destructive mass at T8 level (Figure 7).
Figure 1. Axial contrasted image shows a right spinal soft-tissue mass invading the vertebral body, pedicle, lamina, transverse process, rib, and adjacent pleura. There may be some lung invasion. The mass also extends into the spinal canal, causing significant stenosis.
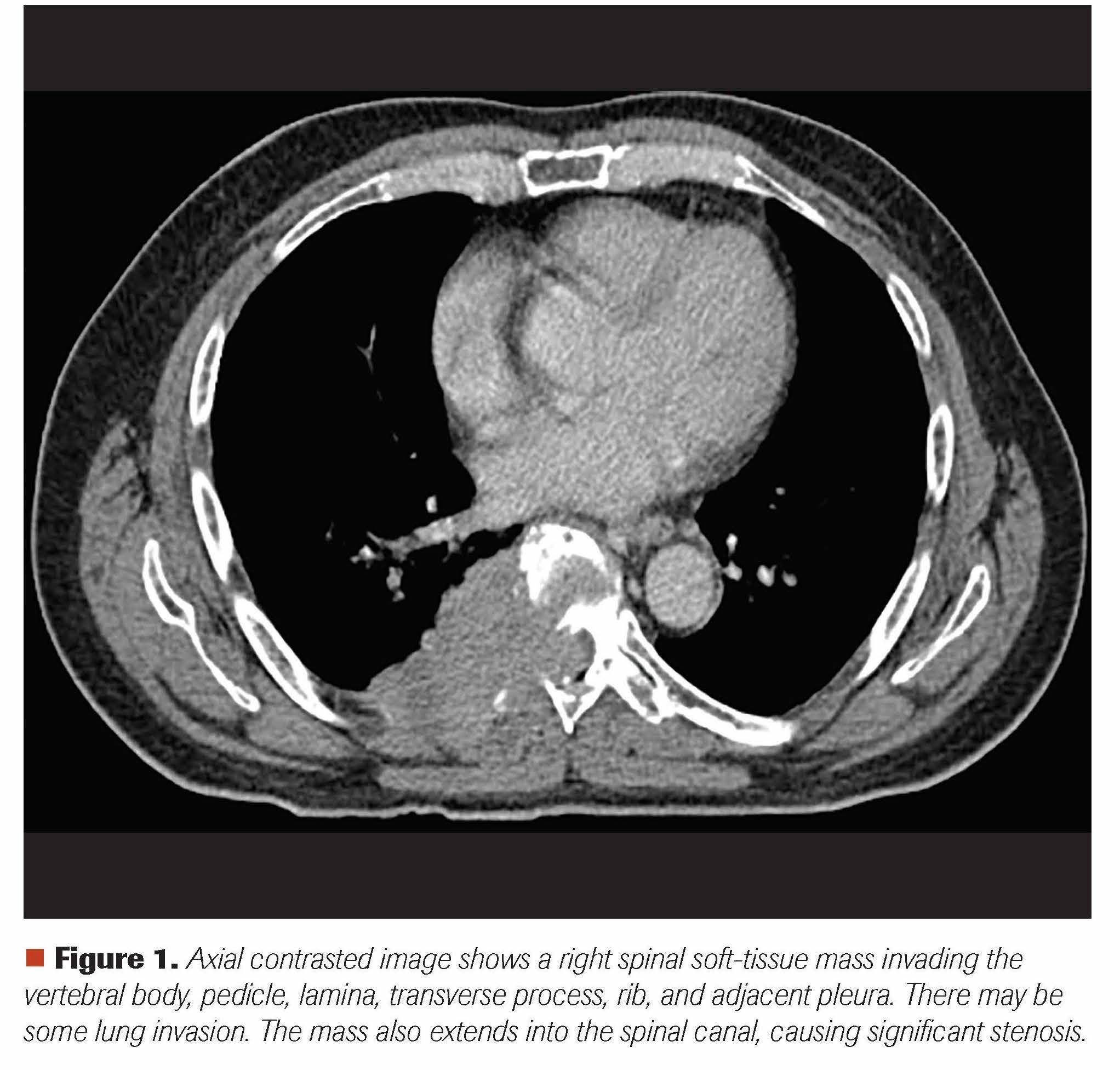
Figure 2. T2 MRI sequence of the mass more easily differentiates the mass from the central canal contents. The interface between the tumor and thecal sac is identified with significant mass effect, severe neural foramen compromise, and moderate-to-severe spinal stenosis. Again seen are the areas of bony invasion as seen on the CT image.
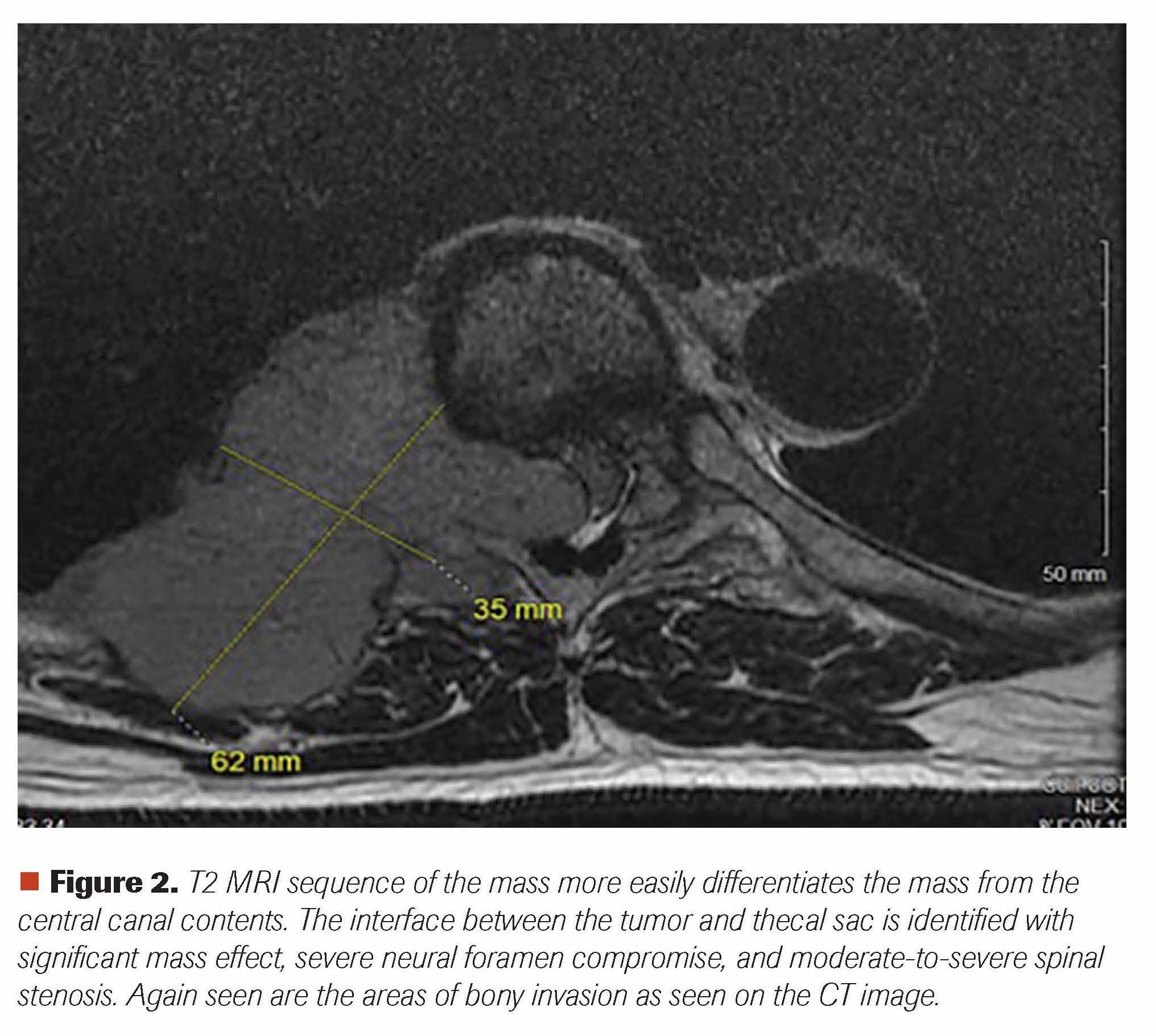
Figure 3 and 4. Spinal mass biopsy showing sheets of plasma cells (hematoxylin and eosin stain, 400x magnification) (left). Spinalmass biopsy showing λ light chain restriction (in situ hybridization for lambda; 400x magnification) (right).
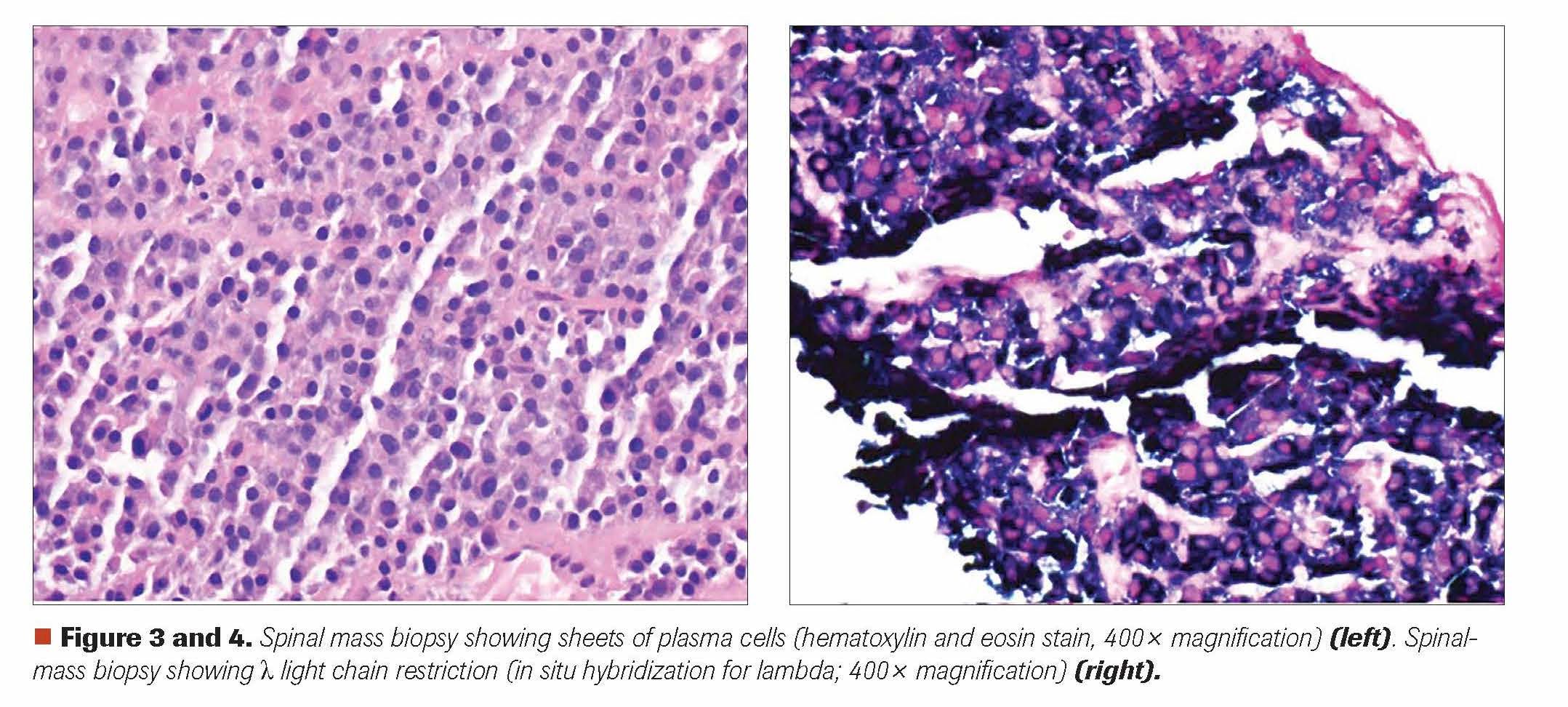
Figure 5 and 6. Bone marrow aspirate showing sheets and clusters of plasma cells (hematoxylin and eosin stain; 400x magnification) (left); Bone marrow aspirate showing lambda light chain restriction (in situ hybridization for lambda; 400x magnification) (right).
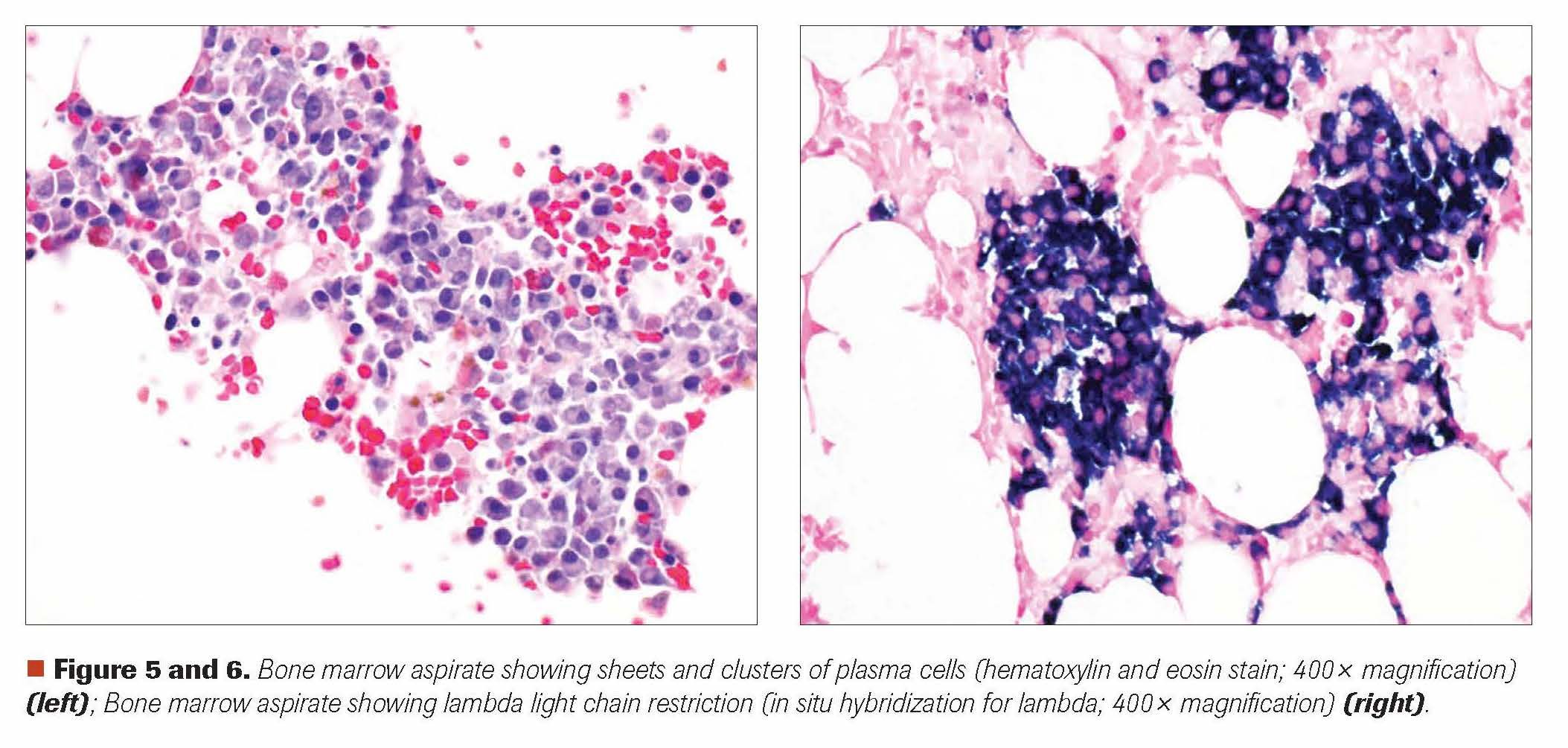
Figure 7. Large osseous destructive mass posterior right hemithorax with prominent destruction of the right posterior eighth rib and adjacent T8 vertebral body. There is likely encroachment into the spinal canal with mass effect upon the thoracic spinal cord.
Discussion
Malignant spinal cord and/or cauda equina compression is a relatively common complication of malignancy. While it is most common in the late stages of cancer, it can be the first manifestation of malignant disease. Depending on the extent and location of the spinal cord involvement, patients may present with various symptoms and signs, ranging from pain and motor and/or sensory loss to paraplegia and urinary or fecal incontinence. Long-term neurological functioning closely correlates with the patient’s mobility at the time of initial presentation. Patients with established spinal cord compression classically exhibit bilateral upper motor neuron findings below the level of the compression, but unilateral findings can also be seen. A circumferential sensory level below which sensation is reduced or altered may be noted. Bowel or bladder dysfunction can be present. In some cases, loss of balance may be the main presenting symptom due to compression of the posterior spinal cord.6,7
Choice of Initial Treatment Modality
The goals of treatment for spinal cord compression are adequate pain control, relief of spinal cord or cauda equina compression, and maintenance of spinal stability, while preserving or improving neurologic function. After the immediate administration of glucocorticoids in nearly all patients, the choice of initial treatment modality depends on several factors, including the presence or absence of spinal instability, the degree of compression of the spinal cord, and the relative radiological and/or chemotherapeutic sensitivity of the tumor.8,9
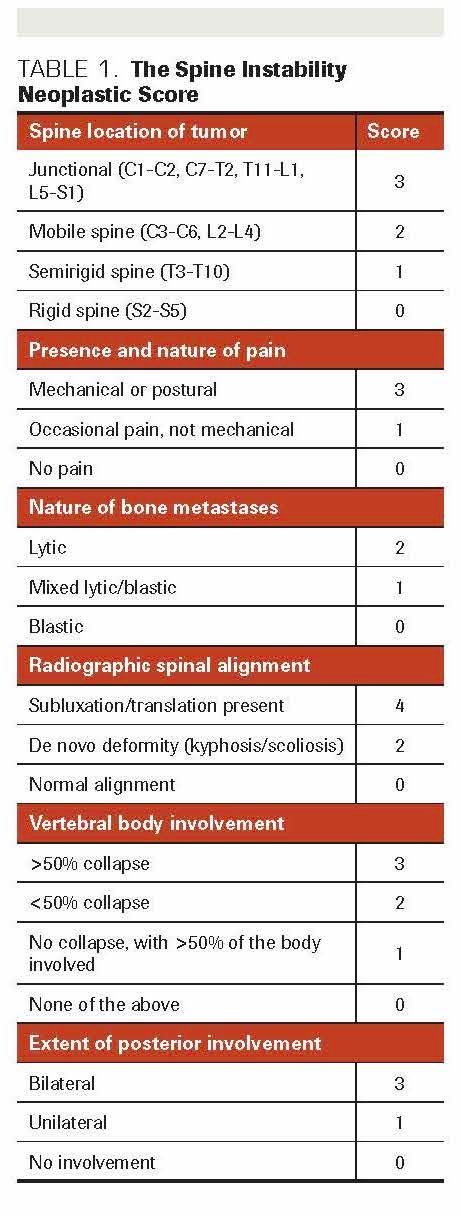
An expert opinion consensus classification system for spinal instability has been developed based on the available evidence about patient symptoms and radiographic criteria.10 This classification uses 6 individual components of spinal instability: spinal location of the tumor, presence and character of the pain, nature of bone metastases, radiographic spinal alignment, extent of vertebral body involvement, and extent of posterior spinal element involvement. All of these are scored to create a final composite Spine Instability Neoplastic Score (SINS) (Table 1).11 In guiding the operative vs nonoperative management of patients with neoplastic spinal cord compression, SINS has been shown to be useful, with very good interobserver agreement among radiologists and radiation oncologists.12,13 According to this classification system, patients with a score of 7 or higher are considered to be at risk for spinal instability. The most appropriate treatment modality for an unstable spine is stabilization either by surgery with fixation14 or by percutaneous vertebral repair.15 RT and spinal bracing have not been shown to be effective for this group of patients.16,17
TABLE 1. The Spine Instability Neoplastic Score
Surgery
A life expectancy of at least 3 months and neurologic function compromise of less than 24 hours have been utilized as indicators for surgical candidacy.18 Patients with hematologic malignancies should be excluded, as they are best managed by RT or chemotherapy. Surgical intervention is performed to accomplish mechanical stabilization, pain relief, preservation of neurological function, and local tumor reduction. Although various surgical approaches can be used, the majority of cases have historically been managed by decompressive pressive posterior laminectomy. However, without instrumentation, decompressive laminectomy has been associated with a failure to resolve anterior compression as well as to cause or exacerbate spinal instability. A stand-alone laminectomy is considered only for metastatic involvement of the epidural space and lamina.
Additionally, the choice of surgical approach—anterior, posterior, or circumferential—is determined by the affected region of the spine. Metastatic spine lesions occurring ventrally in the subaxial cervical spine are best approached anteriorly. For thoracic spine lesions, transpedicular approaches are preferred, because an anterior approach can be challenging due to mediastinal contents. The transpedicular corpectomy and costotransversectomy can provide the added benefit of ventrally decompressing the spinal cord or thecal sac. Costotransversectomy involves more extensive resection and bone removal by providing better access to the anterior spinal column from a more lateral route.19-21 Modern surgical techniques and the development of spinal implants composed of high-quality materials, such as titanium, have significantly improved outcomes.
Prospective evaluations of RT plus laminectomy without instrumentation have not shown any benefit for this combination compared with RT alone.22 Data from prospective cohorts demonstrate that laminectomy combined with instrumentation for stabilization could improve neurological outcomes and pain.23,24 However, these prospective studies do not have control groups, so conclusions are limited. In a select group of patients, surgery followed by RT is a beneficial treatment when compared with RT alone. In a randomized trial, patients with single-level disease, good performance status, and an onset of symptoms within 24 hours were treated with either circumferential decompressive surgery followed by RT (30 Gy in 10 fractions) or RT alone. Analysis showed a clear difference in the number of patients who were able to walk 4 steps post treatment, as well as higher rates of continence and better muscle strength and functional ability, with less need for opioid analgesics and corticosteroids.25 Patients who are not candidates for radical surgery but who have an unstable spine may benefit from minimally invasive techniques such as vertebroplasty and kyphoplasty. Percutaneous vertebroplasty is performed by the percutaneous placement of 1 or 2 trocars into the vertebral bodies through the pedicles, or by the extrapedicular approach and the injection of methylmethacrylate under fluoroscopic guidance. Balloon kyphoplasty is a modified version of percutaneous vertabroplasty; it utilizes an inflatable balloon in a fractured vertebra to create a cavity into which the cement can be injected.26,27
Radiation Therapy
In the absence of compression fracture or instability, external beam RT (EBRT) is also an effective treatment option for patients with significant comorbidities and limited life expectancy. RT is an indispensable part of adjuvant treatment following spine surgery when it was not possible to obtain wide surgical margins. To avoid adversely affecting wound healing, RT should be given 1 to 3 weeks after surgery.28 RT schedules need to be individualized, and efficacy is highly dependent on histology. In general, patients with solid tumors, such as breast and prostate cancers, are moderately radiosensitive, while patients who are mostly radioresistant include those with cancers such as melanoma, osteosarcoma, and thyroid, colon, and renal cancers. RT alone is frequently utilized in patients with such hematological malignancies as lymphoma or myeloma due to the sensitivity of these tumors to RT.29 In a systematic review involving 7 retrospective studies with 885 patients, RT provided a mean local disease control rate of 77%.29 In a meta-analysis involving 543 patients, a pain control rate of 54% to 83% was reported with the use of RT.30
No standard RT regimen exists for the treatment of malignant spinal cord compression. For patients with painful bone metastases, 1 to 5 low-fraction regimens with high single doses (4 to 10 Gy) have been shown to provide similar clinical outcomes to those of more protracted regimens.31-35 In a prospective, randomized, phase 3 trial, Maranazo et al randomized 300 patients to either a short-course (8 Gy x 2 days) or split-course (5 Gy x 3 days or 3 Gy x 5 days) schedule. At a median follow up of 33 months (range, 4-61), both regimens of hypofractionated RT were effective, with no severe adverse effects. Considering the convenience of the short-course regimen, the authors concluded that the short-course therapy could be the hypofractionated RT regimen of choice for patients with malignant spinal cord compression.36
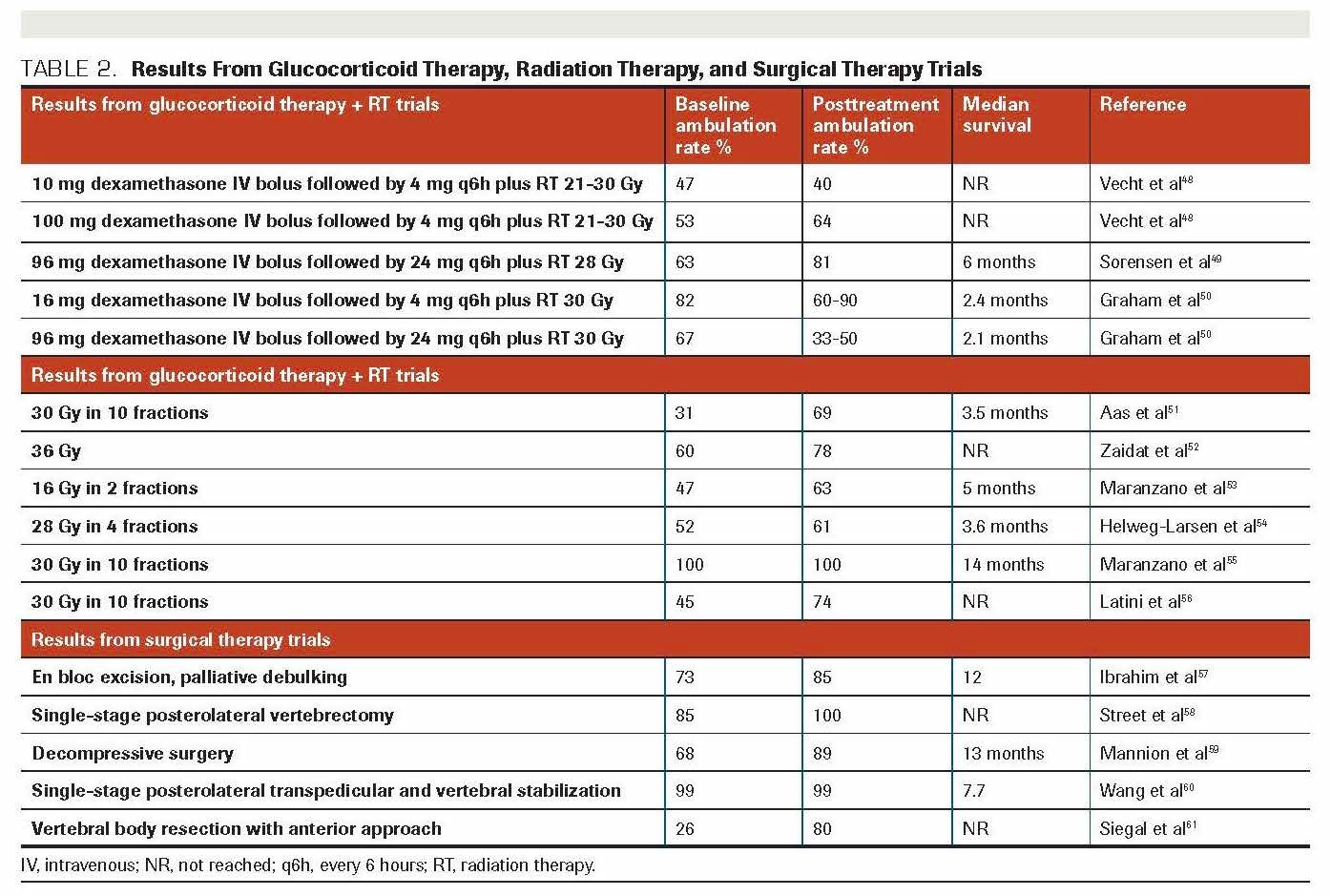
With the advances in stereotactic RT techniques, this approach has been utilized to allow precise high-dose targeting in 1 or 2 fractions while minimizing exposure to the healthy surrounding spinal cord tissue.37 A systematic review involving 59 studies with 5655 patients treated with stereotactic RT for spinal metastases showed local control rates of 80% to 90% for patients with newly diagnosed disease, 80% for postsurgical patients, and 65% for previously radiated patients.38 Results from glucocorticoid therapy, RT, and surgical therapy trials of malignant spinal cord compression are summarized in Table 2.
TABLE 2. Results From Glucocorticoid Therapy, Radiation Therapy, and Surgical Therapy Trials
Spinal Cord Compression in Multiple Myeloma
Multiple myeloma is a clonal B-cell disorder characterized by malignant transformation and the proliferation and accumulation of postgerminal center plasma cells in the bone marrow and occasionally at extramedullary sites. The reported incidence of extramedullary disease in newly diagnosed multiple myeloma ranges from 7% to 18%, while 6% to 20% of patients may develop extramedullary disease later in their disease course.39 The outcomes of patients with multiple myeloma have significantly improved due to the widespread use of autologous stem cell transplantation (ASCT) and novel therapies targeting both the myeloma clone and its microenvironment. Control of bone disease in myeloma patients still represents a therapeutic challenge, however. At some time during their disease course, more than two-thirds of these patients present with osteopenia, osteoporosis, or pathological fractures, which frequently involve the spine and cause spinal cord compression.40
Treatment of spinal lesions in multiple myeloma requires a multidisciplinary approach. Prompt diagnosis and immediate treatment are critically important. Systemic therapy, including such modalities as chemotherapy agents, steroids, proteasome inhibitors, and immunomodulatory drugs, can be used in select patients with minimal risk of neurologic deficit. Surgical management of multiple myeloma–related vertebral lesions is seldom utilized due to this disease’s sensitivity to chemotherapy and RT. The rare indications for surgical intervention may include unstable fractures and spinal cord compression caused by bone fragments protruding from a vertebral fracture.41
The combination of EBRT and glucocorticoids is usually the treatment of choice for multiple myeloma patients who have impending vertebral fracture or spinal cord compression; it also provides pain control. EBRT also represents the treatment of choice for solitary plasmacytomas.42,43 Early studies that were conducted in small patient cohorts demonstrated that pain relief, quality of life, and motor function were improved in a sizable proportion of treated patients.44,45 No differences in general efficacy or in the extent and rapidity of pain relief have been observed using a fractionated 2-week course of 30 Gy vs a single fraction of 8 to 10 Gy.46 The radiation field should be large enough to compensate patient motion but as limited as possible to preserve marrow function. This is especially true for patients who are candidates for ASCT, because peripheral blood stem cell collection can be impaired when RT is applied in large fields.47
Outcome of the Case
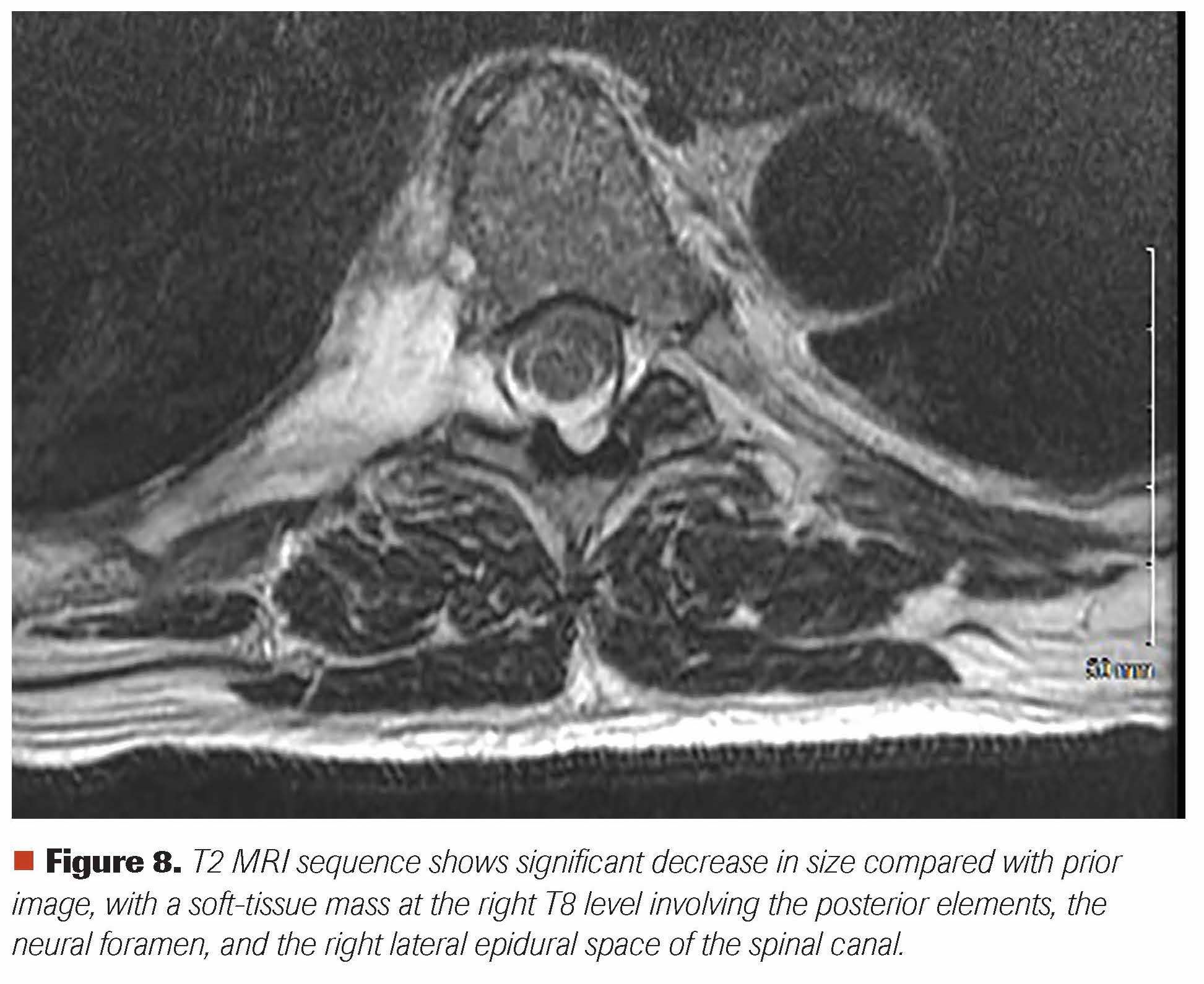
The patient was evaluated by neurosurgery, medical oncology, radiation oncology, and interventional radiology specialties in a multidisciplinary fashion. The SINS was calculated to be 4. He was started on oral dexamethasone along with EBRT to his spinal disease. He received a total of 20 Gy (5 daily fractions of 4 Gy each). Upon completion of his EBRT, he was started on a lenalidomide, bortezomib, and dexamethasone (RVD) regimen. Within the first week of his radiation treatment, he reported a 90% decrease in spinal pain. Five weeks after the start of EBRT, a repeat MRI of the spine showed a significant decrease in spinal mass (Figure 8). Following 2 cycles of RVD, a very good partial response was achieved. After the completion of 4 cycles of RVD, he will be undergoing ASCT with high-dose melphalan chemotherapy.
Figure 8. T2 MRI sequence shows significant decrease in size compared with prior image, with a soft-tissue mass at the right T8 level involving the posterior elements, the neural foramen, and the right lateral epidural space of the spinal canal.
FINANCIAL DISCLOSURE: The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
Copur and Zusag are from the Morrison Cancer Center, Mary Lanning Healthcare, Hastings, Nebraska.
Bell is from the Inspired Brain and Spine Surgery, Mary Lanning Healthcare, Hastings, Nebraska.
Rodriguez is from Diagnostic Radiology, Mary Lanning Healthcare, Hastings, Nebraska.
Wedel and Lintel are from the Pathology Department, Mary Lanning Healthcare, Hastings, Nebraska.
Allan is from Midwest Imaging Interventional Radiology, Grand Island, Nebraska
References:
1.Loblaw DA, Laperriere NJ, Mackillop WJ. A population-based study of malignant spinal cord compression in Ontario. Clin Oncol (R Coll Radiol). 2003;15(4):211-217. doi:10.1016/s0936-6555(02)00400-4
2.National Institute for Health and Care Excellence. Metastatic spinal cord compression: risk assessment, diagnosis and management. clinical guideline [CG75]. November 26, 2008. Accessed August 5, 2014. https://www.nice.org.uk/guidance/CG75/
3.Tsutsumi S, Yasumoto Y, Ito M. Solitary spinal extradural plasmacytoma: a case report and literature review. Clin Neuroradiol. 2013;23(1):5-9. doi:10.1007/s00062-012-0156-z
4.Damaj G, Mohty M, Vey N, et al. Features of extramedullary and extraosseous multiple myeloma: a report of 19 patients from a single center. Eur J Haematol. 2004;73(6):402-406. doi:10.1111/j.1600-0609.2004.00331.x
5.Kyle RA, Gertz MA, Witzig TE, et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc. 2003;78(1):21-33. doi:10.4065/78.1.21
6.Graham Macdonald A, Lynch D, Garbett I, Nazeer N. Malignant spinal cord compression. J R Coll Physicians Edinb. 2019;49(2):151-156. doi:10.4997/JRCPE.2019.217
7.Levack P, Graham J, Collie D, et al; Scottish Cord Compression Study Group. Don’t wait for a sensory level—listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin Oncol (R Coll Radiol). 2002;14(6):472-480. doi:10.1053/clon.2002.0098
8.Skeoch GD, Tobin MK, Khan S, Linninger AA, Mehta AI. Corticosteroid treatment for metastatic spinal cord compression: a review. Global Spine J. 2017;7(3):272-279. doi:10.1177/2192568217699189
9.Lawrie I. Back pain in malignant disease – metastatic spinal cord compression?. Rev Pain. 2010;4(2):14-17. doi:10.1177/204946371000400204
10.Fisher CG, DiPaola CP, Ryken TC, et al. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35(22):E1221-E1229. doi:10.1097/BRS.0b013e3181e16ae2
11.Fourney DR, Frangou EM, Ryken TC, et al. Spinal Instability Neoplastic Score: an analysis of reliability and validity from the Spine Oncology Study Group. J Clin Oncol. 2011;29(22):3072-3077. doi:10.1200/JCO.2010.34.3897
12.Fisher CG, Schouten R, Versteeg AL, et al. Reliability of the Spinal Instability Neoplastic Score (SINS) among radiation oncologists: an assessment of instability secondary to spinal metastases. Radiat Oncol. 2014;9:69. doi:10.1186/1748-717X-9-69
13.Fisher CG, Versteeg AL, Schouten R, et al. Reliability of the Spinal Instability Neoplastic Scale among radiologists: an assessment of instability secondary to spinal metastases. AJR Am J Roentgenol. 2014;203(4):869-874. doi:10.2214/AJR.13.12269
14.Wang JC, Boland P, Mitra N, et al. Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1(3):287-298. doi:10.3171/spi.2004.1.3.0287
15.Mendel E, Bourekas E, Gerszten P, Golan JD. Percutaneous techniques in the treatment of spine tumors: what are the diagnostic and therapeutic indications and outcomes? Spine (Phila Pa 1976). 2009;34(22 Suppl):S93-S100. doi:10.1097/BRS.0b013e3181b77895
16.Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648. doi:10.1016/S0140-6736(05)66954-1
17.Lee SH, Cox KM, Grant R, Kennedy C, Kilbride L. Patient positioning (mobilisation) and bracing for pain relief and spinal stability in metastatic spinal cord compression in adults. Cochrane Database Syst Rev. 2012;(3):CD007609. doi:10.1002/14651858.CD007609.pub2
18.North RB, LaRocca VR, Schwartz J, et al. Surgical management of spinal metastases: analysis of prognostic factors during a 10-year experience. J Neurosurg Spine. 2005;2(5):564-573. doi:10.3171/spi.2005.2.5.0564
19.Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26(3):298-306. doi:10.1097/00007632-200102010-00016
20.Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005;30(19):2186-2191. doi:10.1097/01.brs.0000180401.06919.a5
21.Molina C, Goodwin CR, Abu-Bonsrah N, Elder BD, de la Garza Ramos R, Sciubba DM. Posterior approaches for symptomatic metastatic spinal cord compression. Neurosurg Focus. 2016;41(2):E11. doi:10.3171/2016.5.FOCUS16129
22.Rades D, Huttenlocher S, Bajrovic A, et al. Surgery followed by radiotherapy versus radiotherapy alone for metastatic spinal cord compression from unfavorable tumors. Int J Radiat Oncol Biol Phys. 2011;81(5):e861-e868. doi:10.1016/j.ijrobp.2010.11.056
23.Young RF, Post EM, King GA. Treatment of spinal epidural metastases. randomized prospective comparison of laminectomy and radiotherapy. J Neurosurg. 1980;53(6):741-748. doi:10.3171/jns.1980.53.6.0741
24.Fuentes S, Métellus P, Pech-Gourg G, Adetchessi T, Dufour H, Grisoli F. Open kyphoplasty for management of metastatic spine fracture [article in French]. Neurochirurgie. 2007;53(2-3 Pt 1):49-53. doi:10.1016/j.neuchi.2007.04.001
25.Patchell RA, Tibbs PA, Regine WF, et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet. 2005;366(9486):643-648. doi:10.1016/S0140-6736(05)66954-1
26.Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg. 2003;98(1 Suppl):21-30. doi:10.3171/spi.2003.98.1.0021
27.Chen F, Xia Y-H, Cao W-Z, et al. Percutaneous kyphoplasty for the treatment of spinal metastases. Oncol Lett. 2016;11(3):1799-1806. doi:10.3892/ol.2016.4121
28.Itshayek E, Yamada J, Bilsky M, et al. Timing of surgery and radiotherapy in the management of metastatic spine disease: a systematic review. Int J Oncol. 2010;36(3):533-544.
29.Gerszten PC, Mendel E, Yamada Y. Radiotherapy and radiosurgery for metastatic spine disease: what are the options, indications, and outcomes? Spine (Phila Pa 1976). 2009;34(22 Suppl):S78-S92. doi:10.1097/BRS.0b013e3181b8b6f5
30.Klimo P Jr, Thompson CJ, Kestle JRW, Schmidt MH. A meta-analysis of surgery versus conventional radiotherapy for the treatment of metastatic spinal epidural disease. Neuro Oncol. 2005;7(1):64-76. doi:10.1215/S1152851704000262
31.Cole DJ. A randomized trial of a single treatment versus conventional fractionation in the palliative radiotherapy of painful bone metastases. Clin Oncol (R Coll Radiol). 1989;1(2):59-62. doi:10.1016/s0936-6555(89)80035-4
32.Hoskin PJ, Price P, Easton D, et al. A prospective randomised trial of 4 Gy or 8 Gy single doses in the treatment of metastatic bone pain. Radiother Oncol. 1992;23(2):74-78. doi:10.1016/0167-8140(92)90338-u
33.Steenland E, Leer JW, van Houwelingen H, et al. The effect of a single fraction compared to multiple fractions on painful bone metastases: a global analysis of the Dutch Bone Metastasis Study. Radiother Oncol. 1999;52(2):101-109. doi:10.1016/s0167-8140(99)00110-3. Published correction appears in Radiother Oncol. 1999;53(2):167.
34.Wu JS-Y, Wong R, Johnston M, Bezjak A, Whelan T; Cancer Care Ontario Practice Guidelines Initiative Supportive Care Group. Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J Radiat Oncol Biol Phys. 2003;55(3):594-605. doi:10.1016/s0360-3016(02)04147-0
35.van den Hout WB, van der Linder YM, Steenland R, et al. Single- versus multiple-fractionation radiotherapy in patients with painful bone metastases: cost-utility analysis based on randomized trial. J Natl Cancer Inst. 2003;95(3):222-229. doi:10.1093/jnci/95.3.222
36.Maranzano E, Bellavita R, Rossi R, et al. Short-course versus split-course radiotherapy in metastatic spinal cord compression: results of a phase III, randomized, multicenter trial. J Clin Oncol. 2005;23(15):3358-3365. doi:10.1200/JCO.2005.08.193
37.Redmond KJ, Robertson S, Lo SS, et al. Consensus contouring guidelines for postoperative stereotactic body radiation therapy for metastatic solid tumor malignancies to the spine. Int J Radiat Oncol Biol Phys. 2017;97(1):64-74. doi:10.1016/j.ijrobp.2016.09.014
38.Glicksman RM, Tjong MC, Neves-Junior WFP, et al. Stereotactic ablative radiotherapy for the management of spinal metastases: a review. JAMA Oncol. 2020;6(4):567-577. doi:10.1001/jamaoncol.2019.5351. Published correction appears in JAMA Oncol. 2020;6(8):1303.
39.Bladé J, Fernández de Larrea C, Rosiñol L. Extramedullary involvement in multiple myeloma. Haematologica. 2012;97(11):1618-1619. doi:10.3324/haematol.2012.078519
40.Lecouvet FE, Vande Berg BC, Maldague BE, et al. Vertebral compression fractures in multiple myeloma. part I. distribution and appearance at MR imaging. Radiology. 1997;204(1):195-199. doi:10.1148/radiology.204.1.9205246
41.Utzschneider S, Schmidt H, Weber P, Schmidt GP, Jansson V, Dürr HR. Surgical therapy of skeletal complications in multiple myeloma. Int Orthop. 2011;35(8):1209-1213. doi:10.1007/s00264-010-1127-0
42.Knobel D, Zouhair A, Tsang RW, et al; Rare Cancer Network. Prognostic factors in solitary plasmacytoma of the bone: a multicenter Rare Cancer Network study. BMC Cancer. 2006;6:118. doi:10.1186/1471-2407-6-118
43.Huang W, Cao D, Ma J, et al. Solitary plasmacytoma of cervical spine: treatment and prognosis in patients with neurological lesions and spinal instability. Spine (Phila Pa 1976). 2010;35(8):E278-E284. doi:10.1097/BRS.0b013e3181c9b431
44.Lecouvet F, Richard F, Vande Berg B, et al. Long-term effects of localized spinal radiation therapy on vertebral fractures and focal lesions appearance in patients with multiple myeloma. Br J Haematol. 1997;96(4):743-745. doi:10.1046/j.1365-2141.1997.d01-2108.x
45.Balducci M, Chiesa S, Manfrida S, et al. Impact of radiotherapy on pain relief and recalcification in plasma cell neoplasms: long-term experience. Strahlenther Onkol. 2011;187(2):114-119. doi:10.1007/s00066-010-2155-9
46.Balducci M, Chiesa S, Manfrida S, et al. Impact of radiotherapy on pain relief and recalcification in plasma cell neoplasms: long-term experience. Strahlenther Onkol. 2011;187(2):114-119. doi:10.1007/s00066-010-2155-9
47.Olivieri A, Marchetti M, Lemoli R, et al. Proposed definition of ‘poor mobilizer’ in lymphoma and multiple myeloma: an analytic hierarchy process by ad hoc working group Gruppo ItalianoTrapianto di Midollo Osseo. Bone Marrow Transplant. 2012;47(3):342-351. doi:10.1038/bmt.2011.82
48.Vecht CJ, Haaxma-Reiche H, van Putten WL, de Visser M, Vries EP, Twijnstra A. Initial bolus of conventional versus high-dose dexamethasone in metastatic spinal cord compression. Neurology. 1989;39(9):1255-1257. doi:10.1212/wnl.39.9.1255
49.Sørensen S, Helweg-Larsen S, Mouridsen H, Hansen HH. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer. 1994;30A(1):22-27. doi:10.1016/s0959-8049(05)80011-5
50.Graham PH, Capp A, Delaney G, et al. A pilot randomised comparison of dexamethasone 96 mg vs 16 mg per day for malignant spinal-cord compression treated by radiotherapy: TROG 01.05 Superdex study. Clin Oncol (R Coll Radiol). 2006;18(1):70-76. doi:10.1016/j.clon.2005.08.015
51.Aass N, Fosså SD. Pre- and post-treatment daily life function in patients with hormone resistant prostate carcinoma treated with radiotherapy for spinal cord compression. Radiother Oncol. 2005;74(3):259-265. doi:10.1016/j.radonc.2004.12.001
52.Zaidat OO, Ruff RL. Treatment of spinal epidural metastasis improves patient survival and functional state. Neurology. 2002;58(9):1360-1366. doi:10.1212/wnl.58.9.1360
53.Maranzano E, Latini P, Perrucci E, Beneventi S, Lupattelli M, Corgna E. Short-course radiotherapy (8 Gy x 2) in metastatic spinal cord compression: an effective and feasible treatment. Int J Radiat Oncol Biol Phys. 1997;38(5):1037-1044. doi:10.1016/s0360-3016(97)00128-4
54.Helweg-Larsen S. Clinical outcome in metastatic spinal cord compression. a prospective study of 153 patients. Acta Neurol Scand. 1996;94(4):269-275. doi:10.1111/j.1600-0404.1996.tb07064.x
55.Maranzano E, Latini P, Beneventi S, et al. Radiotherapy without steroids in selected metastatic spinal cord compression patients. a phase II trial. Am J Clin Oncol. 1996;19(2):179-183. doi:10.1097/00000421-199604000-00018
56.Latini P, Maranzano E, Ricci S, et al. Role of radiotherapy in metastatic spinal cord compression: preliminary results from a prospective trial. Radiother Oncol. 1989;15(3):227-233. doi:10.1016/0167-8140(89)90090-x
57.Ibrahim A, Crockard A, Antonietti P, et al. Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? an international multicenter prospective observational study of 223 patients. invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine. 2008;8(3):271-278. doi:10.3171/SPI/2008/8/3/271
58.Street J, Fisher C, Sparkes J, et al. Single-stage posterolateral vertebrectomy for the management of metastatic disease of the thoracic and lumbar spine: a prospective study of an evolving surgical technique. J Spinal Disord Tech. 2007;20(7):509-520. doi:10.1097/BSD.0b013e3180335bf7
59.Mannion RJ, Wilby M, Godward S, Lyratzopoulos G, Laing RJC. The surgical management of metastatic spinal disease: prospective assessment and long-term follow-up. Br J Neurosurg. 2007;21(6):593-598. doi:10.1080/02688690701593579
60.Wang JC, Boland P, Mitra N, et al. Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction: results in 140 patients. invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1(3):287-298. doi:10.3171/spi.2004.1.3.0287
61.Siegal T, Tiqva P, Siegal T. Vertebral body resection for epidural compression by malignant tumors. results of forty-seven consecutive operative procedures. J Bone Joint Surg Am. 1985;67(3):375-382.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.