Phase II Trial of Weekly Irinotecan/Cisplatin in Advanced Esophageal Cancer
Esophageal cancer is a rare but highly virulent malignancy in theUnited States, and adenocarcinoma of the esophagus has had the mostrapid rate of increase of any solid tumor malignancy. Systemic metastaticdisease is present in 50% of patients at diagnosis. In the remaining50% presenting with local regional disease, systemic metastatic diseasewill develop in the vast majority of these patients.
Esophageal cancer is a rare but highly virulent malignancy in the United States, and adenocarcinoma of the esophagus has had the most rapid rate of increase of any solid tumor malignancy. Systemic metastatic disease is present in 50% of patients at diagnosis. In the remaining 50% presenting with local regional disease, systemic metastatic disease will develop in the vast majority of these patients. The limited efficacy and toxicity of conventional fluorouracil (5-FU)/cisplatin–based chemotherapy has prompted the evaluation of newer agents. Irinotecan (Camptosar) has shown promising single-agent activity in a number of gastrointestinal cancers, including colorectal, pancreatic, and esophagogastric cancer. The phase II evaluation of the combination of weekly irinotecan and cisplatin has shown encouraging response rates exceeding 30% to 50% in esophageal and gastric cancer. Hematologic toxicity using a schedule of 4 consecutive weeks of therapy followed by 2 weeks of rest prompted interest in a multicenter trial evaluation of a change in therapy delivery to 2 weeks on and 1 week off. Cisplatin at 30 mg/m2 was administered with irinotecan at 65 mg/m2, days 1 and 8, on an every-21-day schedule. Thirty-nine patients were entered on study, with 36 evaluable for toxicity and 31 evaluable for response. Grade 3/4 neutropenia was observed in only 22% of patients, reduced from 49% in a prior phase II trial employing 4 consecutive weeks of therapy. Confirmed major responses were observed in 36% of patients (10 of 28). A change to a day 1, day 8 schedule of weekly irinotecan and cisplatin appears to reduce hematologic toxicity but maintain antitumor activity in patients with esophageal and gastroesophageal junction cancer. A randomized phase II trial in gastric and esophageal cancer comparing weekly irinotecan and cisplatin to epirubicin, cisplatin, and 5-FU, and to infusional 5-FU in combination with irinotecan, will be conducted by the Cancer and Leukemia Group B (CALGB). A phase II trial combining this schedule of weekly cisplatin and irinotecan and concurrent radiotherapy given as preoperative therapy will also be conducted by the CALGB as a pilot trial.
Esophageal carcinoma is an aggressive cancer with a poor prognosis. In 2004, it is estimated that 14,250 Americans will be diagnosed with esophageal cancer, and more than 90% of these patients will die of their disease.[1] Half of patients present with overt metastatic disease, with a median survival of usually less than 1 year. The remaining half present with locally advanced disease potentially amenable to treatment with surgery or radiation-based therapy.
Because of the relative rarity of esophageal cancer and the absence of effective screening, most patients present with symptomatic dysphagia and usually have locally advanced, transmural, or lymph node-positive disease. Despite treatment with surgery, definitive chemoradiotherapy, or the combined use of preoperative chemoradiotherapy followed by surgery, a 5-year survival of less than 20% to 35% is generally achieved.[2- 5] The poor survival in locally advanced disease is due to a high incidence of distant metastatic recurrence of disease as well as a significant incidence of local recurrence of disease.
The toxicity of conventionally used chemotherapy combining a continuous infusion of fluorouracil (5-FU) and cisplatin is substantial-it includes stomatitis, diarrhea, nausea, fatigue, and myelosuppression. The limited effectiveness and toxicity of currently used cytotoxic chemotherapy, either to palliate metastatic disease or when used in combination with radiotherapy in locally advanced disease, have mandated the ongoing investigation of newer cytotoxic agents in esophageal cancer.
Irinotecan
TABLE 1

Phase II Trial of Day 1, Day 8 Cisplatin and Irinotecan: Demographics
Irinotecan (Camptosar) is a semisynthetic camptothecin that inhibits topoisomerase , an enzyme required to uncoil DNA during DNA synthesis and repair. Irinotecan has emerged as a significant new cytotoxic agent with a broad spectrum of antitumor activity. Early trials in Japan indicated promising antitumor activity for irinotecan in a number of gastrointestinal malignancies, including colorectal, pancreatic, and gastric cancer. Phase II evaluation of irinotecan in gastric cancer in Japan indicated a singleagent response rate of 20% to 30%.[6] Recent American trials of single-agent irinotecan, given at a weekly dose of 125 mg/m2, 4 weeks on and 2 weeks off, indicate modest single-agent activity with a response rate of 15% in gastric and gastroesophageal junction cancer.[7,8]
At the Memorial Sloan-Kettering Cancer Center, Saltz et al developed a weekly schedule of cisplatin and irinotecan to optimize potential synergy between the two agents.[9] Neutropenia was the main dose-limiting toxicity. Other toxicities, which included manageable diarrhea, nausea, and fatigue, were minimal. The phase II doses for previously untreated patients were identified as 30 mg/m2 for cisplatin and 65 mg/m2 for irinotecan.
Ilson and colleagues subsequently performed a phase II trial of weekly cisplatin and irinotecan in metastatic esophageal cancer using the schedule developed by Saltz.[10] The primary end point was antitumor response rate. Secondary end points included assessment of relief of dysphagia with chemotherapy, and the impact of therapy on quality of life as measured by the Functional Assessment of Cancer Therapy-General (FACT-G) scale and the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Questionnaire (QLQ) C-30.
A remarkable response rate of 57% was observed in 35 patients, with comparable responses in adenocarcinoma and squamous cell carcinoma. The median duration of response was 4.2 months, and the median actuarial survival was 14.6 months. Dysphagia relief- either improvement or resolution of dysphagia-was achieved in 90% of patients. Quality-of-life indices showed significant improvement in responding patients. Therapy was well tolerated. However, grade 3/4 neutropenia was seen in 46% of patients, although it was predominantly grade 3 (37%). Treatment delays due to prolonged recovery of blood counts were common and affected 66% of patients. Most commonly, a delay occurred in week 3 or 4 of therapy; less commonly, there was a shortening of the treatment cycle from 4 to 3 weeks.
A confirmatory trial of the weekly Saltz regimen conducted in metastatic gastric and gastroesophageal junction cancer was recently reported by Ajani and colleagues at the M. D. Anderson Cancer Center.[11] An overall response rate of 54% was re- ported in 39 patients treated. Frequent delays in therapy due to hematologic toxicity were also reported on this trial.
Phase II Multicenter Trial of Day 1, Day 8 Cisplatin/Irinotecan
Because of the need for a delay in therapy with weekly irinotecan and cisplatin using 4 consecutive weeks of therapy, a change in the schedule of weekly therapy to a 2-week-on, 1-week-off schedule was proposed. A phase II multicenter trial exploring this alternative schedule has recently been completed and reported in abstract form.[12] Patients with metastatic or unresectable esophageal cancer or cancer of the gastroesophageal junction were eligible if they had received no prior chemotherapy and if they had measurable disease by the RECIST criteria.
FIGURE 1

Treatment Dosage and Schedule
Thirty-nine patients were enrolled from 14 participating centers. Patient demographics are outlined in Table 1. The median Eastern Cooperative Oncology Group performance status was 1, and the majority of patients had adenocarcinoma (74%), metastatic disease (85%), and hepatic metastases (64%). The treatment schema is outlined in Figure 1. Patients received cisplatin at 30 mg/m2 by bolus infusion, followed by irinotecan at 65 mg/m2 administered over a 30- minute infusion. Patients were treated in the outpatient setting with hydration and antiemetic prophylaxis with 5-HT3 antagonists and dexamethasone given orally or intravenously.
TABLE 2
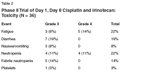
Phase II Trial of Day 1, Day 8 Cisplatin and Irinotecan: Toxicity (N = 36)
Toxicity of treatment in 36 evaluable patients is outlined in Table 2. Therapy was generally well tolerated, with only seven patients having grade 3 diarrhea (19%) and with no patients having grade 4 diarrhea. Nausea and vomiting were uncommon using a schedule of weekly low-dose cisplatin, and grade 3 nausea or vomiting occurred in only three patients (8%). Hematologic toxicity was also tolerable, with grade 3 or 4 neutropenia occurring in only 22% of patients and febrile neutropenia in five patients (13%). Therapy delay, or the elimination of a week of treatment, affected only nine patients (25%). Ninety-three percent of planned cisplatin doses were administered; 92% of irinotecan doses were administered.
TABLE 3

Phase II Trial of Day 1, Day 8 Cisplatin and Irinotecan: Response
Response to therapy in 31 evaluable patients is outlined in Table 3. Confirmed partial responses were observed in 36% of patients (10 of 28 patients), with three additional partial responses awaiting confirmation (an unconfirmed partial response rate of 42%).
Conclusions
The change in schedule of weekly irinotecan and cisplatin in metastatic esophageal cancer from a 4-week-on, 2-week-off schedule to a day 1, day 8 schedule administered every 21 days resulted in a lessening of hematologic toxicity and a reduction in the number of therapy delays and missed treatments. Antitumor response in a multicenter phase II trial seems to have been maintained despite a change in treatment schedule.
The dose and schedule of weekly irinotecan and cisplatin used in this trial will now be evaluated in a trial conducted by the Cancer and Leukemia Group B (CALGB) in advanced gastric and esophageal cancer, comparing this therapy to a combination of infusional 5-FU and irinotecan, and to the regimen of epirubicin, cisplatin, and continuous infusion 5-FU, a standard regimen developed in the United Kingdom. The tolerance and ease of administration of this regimen indicate that it may be a treatment platform to add other agents, or to combine with concurrent radiotherapy.
A recently reported phase I trial combining weekly irinotecan and cisplatin with radiation therapy in esophageal cancer indicates good patient tolerance of therapy and relatively minimal therapy-related toxicity.[13] The CALGB will also evaluate the use of irinotecan, cisplatin, and concurrent radiation in a preoperative pilot trial in locally advanced esophageal cancer.
Financial Disclosure:Dr. Ilson has received research grant support from Pfizer and Aventis. He has served on speakers’ bureaus for Pfizer, Aventis, Roche, and Genentech.
References:
1. Jemal A, Tiwari RC, Murray T, et al: Cancer statistics, 2004. CA Cancer J Clin 54:8- 29, 2004.
2. Walsh TN, Noonan N, Hollywood D, et al: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335:462-467, 1996.
3. Kelsen DP, Ginsberg R, Pajak T, et al: Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339:1979-1984, 1998.
4. Cooper J, Guo M, Herskovic A, et al: Chemoradiotherapy of locally advanced esophageal cancer: Long-term follow-up of a prospective randomized trial (RTOG 85-01). JAMA 281:1623-1627, 1999.
5. Urba SG, Orringer MB, Turrisi A, et al: Randomized trial of preoperative chemo radiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19:305-313, 2001.
6. Kambe M, Wakui A, Nakao I, et al: A late phase II study of irinotecan in patients with advanced gastric cancers (abstract). Proc Am Soc Clin Oncol 12:584, 1993.
7. Lin L, Hecht JR: A phase II trial of irinotecan in patients with advanced adenocarcinoma of the gastroesophageal (GE) junction (abstract 1130). Proc Am Soc Clin Oncol 19:289a, 2000.
8. Enzinger PC, Kulke MH, Clark JW, et al: Phase II trial of CPT-11 in previously untreated patients with advanced adenocarcinoma of the esophagus and stomach (abstract 1243). Proc Am Soc Clin Oncol 19:315a, 2000.
9. Saltz L, Spriggs D, Schaaf L, et al: Phase I clinical and pharmacologic study of weekly cisplatin combined with weekly irinotecan (CPT-11) in patients with advanced solid tu mors. J Clin Oncol 16:3858-3865, 1998.
10. Ilson DH, Saltz L, Enzinger P, et al: Phase II trial of weekly irinotecan plus cisplatin in advanced esophageal cancer. J Clin Oncol 17:3270-3275, 1999.
11. Ajani J, Baker J, Pisters P, et al: CPT-11 plus cisplatin in patients with advanced, untreated gastric or gastroesophageal junction carcinoma: Results of a phase II study. Cancer 94:641-646, 2002.
12. Ilson D, Graham C, Steinbrenner L, et al: A multicenter phase II trial of weekly irinotecan and cisplatin in advanced esophageal and GE junction cancer (abstract 1111). Proc Am Soc Clin Oncol 22:277, 2003.
13. Ilson D, Bains M, Kelsen D, et al: Phase I trial of escalating-dose irinotecan given weekly with cisplatin and concurrent radiotherapy in locally advanced esophageal cancer. J Clin Oncol 21:2926-2932, 2003.